In this blog post, we are discussing ADLs (Activities of Daily Living) for kids and teens. These occupational self care tasks are tasks that make up day to day living. Let’s break this down. For additional information on various roles, check out our article on IADLs.
Occupational self care refers to many things. Occupational therapy practitioners support individuals with daily activities that are part of a functional life. One of those important daily tasks is personal self-care, or the ability to care for one’s own being. From dressing oneself to toileting, all of these include daily occupational self care tasks.
In this blog post, you’ll find resources and activities to support children of all abilities in self-care skills.

When exploring the topic of occupational self care, you’ll also want to check out our resource on developmental checklist as a tool for understanding typical development of skill acquisition.
ADLs are self-care skills
Self-care skills, also known as Activities of Daily Living (ADLs), are essential tasks that individuals of all ages perform to take care of their own physical, emotional, and mental well-being.
For children, occupational performance in ADLs is dependent on the child’s age and stage. We can take a look at various stages of development with regard to ADL participation. Those stages include:
- infancy
- toddlerhood
- early childhood
- elementary childhood
- adolescense
- adulthood
Each of these stages will involve different components and abilities when it comes to occupational performance and ADL skills. You will see and expect different occupational roles, adaptive behaviors, self-care skills and abilities, and changes in self-management needs.
Infant Self-Care Skills
Infant self-care involves receiving nurturance of parents and guardians. Self-sufficiency involves primitive reflexes and accepting self-care. ADLs in the infancy stage is mainly regarding family participation which is a vital role.
The infant responds to nurturing, and takes nourishment they receive from their parent or caregiver. They are learning to move and communicate. During the infant stage, babies gain control of their body as they learn to move in daily self-care tasks.
Toddler Self-Care Skills
For toddlers, self-care continues to involve acceptance of the self-care routines provided by parents or guardians. However, at this age, there is more independence beginning as well. You’ll see preference and willingness in toddler ADLs.
Toddlers are refining and mastering some of the skills that they have passively participated in during the first 2 years of their life.
They start to develop self-sufficiency in eating, dressing, washing, and toileting areas.
Childhood Self-Care Skills
During the ages of 6-12, children have continued occupational roles as a daughter or son, friend, and now as a student. These new roles with peers bring on additional self-care tasks as well as adaptive behaviors in childhood ADLs.
The self-care skills of a child include continuing to master ADL skills with more self-sufficiency, routine participation (brushing their teeth each morning and evening with greater independence) and less support.
Children develop preferences in expressing themselves in hairstyles and clothing, which impacts self-care. There are also new learning opportunities which impact occupational performance, including social skills and peer interaction.
Refer to our blog post on occupational therapy for middle school for the end range of this stage.
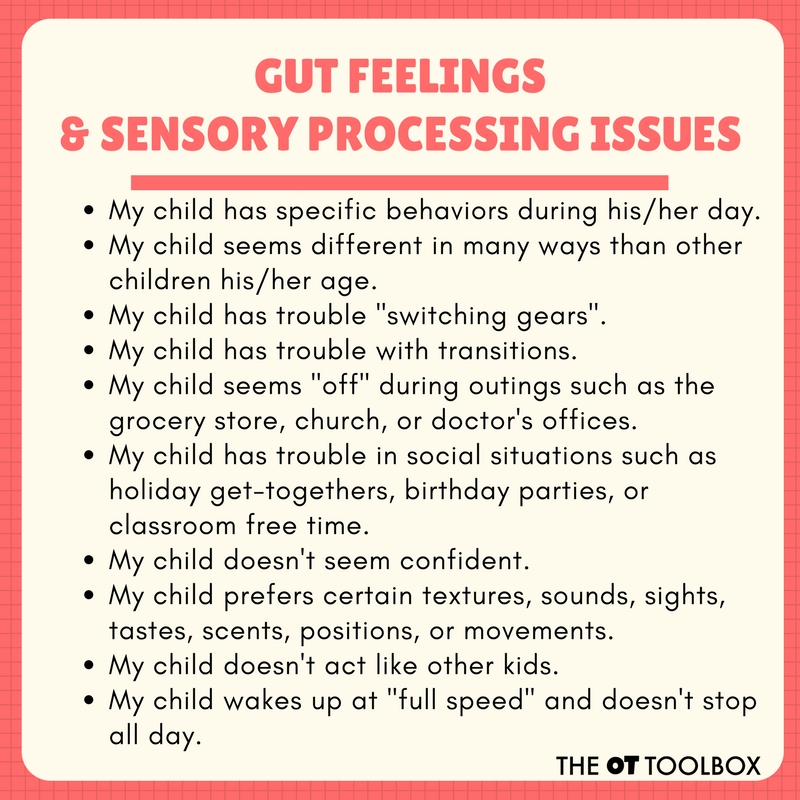
Adolescence and Self-Care
The years between ages 13 and 19 bring on even more development and self-sufficiency during adolescence. They also have more occupational roles such as an employee, a driver on the road, a teammate, volunteer, and may have a different peer group than before.
Self-care, and ALDs in the teen years include mastery or independence of ADLs and IADLs. There is self-expression, building relationships, and defining occupational roles involved in this stage. The adolescence is preparing for independent living, so self-care supports that transition.
Check out our bog post on occupational therapy for teens for more information.
Occupational therapy practitioners are skilled in analyzing, evaluating, and creating detailed plans of care of ADLs at all stages of life.
What are ADLs?
Activities of Daily Living (ADLs) are daily tasks, or activities, that make up a person’s day. They are tasks that are required for participating (or living) in an environment such as a home or workplace. ADLs involve occupational roles or the various roles one plays throughout their day.
These skills are fundamental for daily life and can vary depending on a person’s age and abilities.
Activities of Daily Living Examples
Self-care skills encompass a wide range of activities and typically include:
- Personal hygiene
- Bathing or showering: The ability to clean one’s body, including washing hair, face, and body.
- Oral care: Brushing teeth, flossing, and mouthwash.
- Hair care: Brushing hair, combing, and washing hair with shampoo and conditioner
- Grooming- hair care, shaving, hygiene
- Makeup application
- Washing face
- Caring for hair styles including using a ponytail holder, styling hair, etc.
- Handwashing: Proper handwashing techniques to maintain hygiene.
- Dressing and clothing management
- Dressing: Putting on and taking off clothing, including clothing fasteners like buttons and zippers.
- Selecting appropriate clothing: Choosing weather-appropriate clothing and outfits suitable for different occasions.
- Putting on and tying shoes or fastening shoes
- Nutrition and meal preparation
- Eating independently: Holding utensils to eat, using utensils, drinking from a cup, and managing food.
- Meal preparation: Basic cooking skills, such as preparing simple meals or snacks.
- Toileting and Bathroom Skills
- Using the toilet: Going to the toilet independently, managing clothing, and proper wiping and perineal hygiene skills
- Toilet training: Learning to use the toilet for children.
- Mobility and transfers
- Safety skills in daily tasks
- Awareness of danger: Recognizing and responding to potential hazards.
- Emergency procedures: Knowing what to do in emergencies, such as fire drills or safety protocols.
- Medication management
- Taking medications: The ability to take prescribed medications independently and follow dosing instructions.
- Time management and organization to participate in daily tasks
- Scheduling: Managing daily routines, appointments, and activities.
- Staying on task: Using calendars, reminders, or tools to stay organized.
- Transferring or mobility in daily tasks, like moving from one surface to another, sitting and standing from the toilet, getting into and out of a car, moving in and out of the shower or bathtub, getting into and out of bed, sitting and standing from various surfaces and seats. All of these are considered functional mobility in ADLs.
Self-care skills are crucial for promoting independence, maintaining health, and participating in daily life. These skills are typically learned and developed throughout childhood and adolescence, and they may need to be adapted or supported as individuals age or face physical or cognitive challenges.
Occupational Self-Care
Occupational therapy professionals often work with individuals to enhance or regain occupational self-care skills as part of rehabilitation or therapeutic interventions.
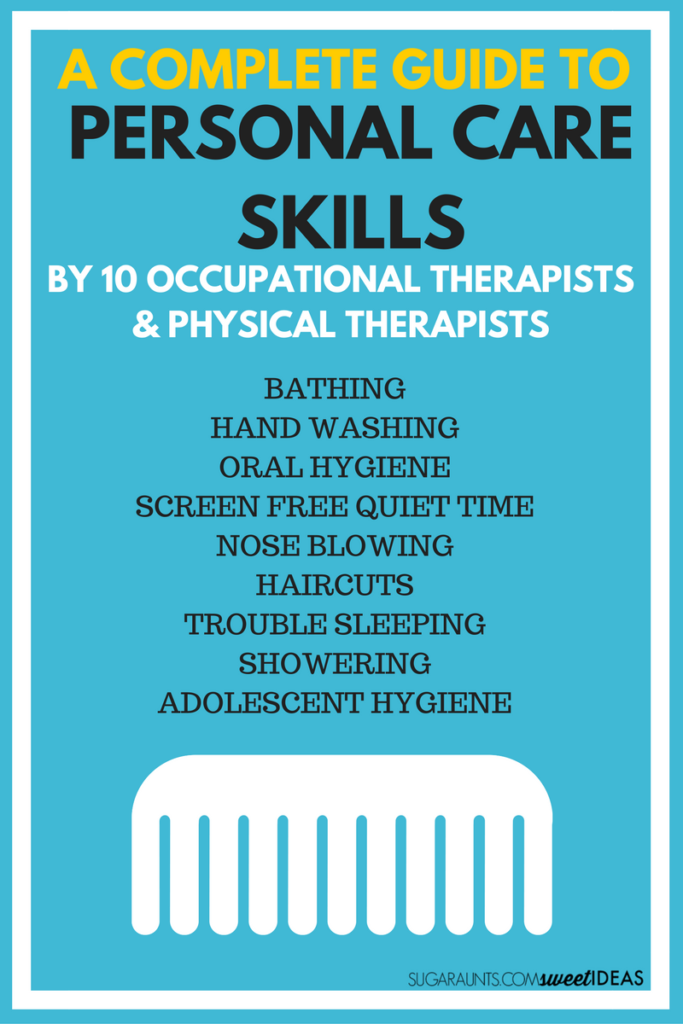
How to Help Kids Learn Self Care and Personal Care Skills:
Adolescent Hygiene Challenges | Therapy Fun Zone

Colleen Beck, OTR/L has been an occupational therapist since 2000, working in school-based, hand therapy, outpatient peds, EI, and SNF. Colleen created The OT Toolbox to inspire therapists, teachers, and parents with easy and fun tools to help children thrive. Read her story about going from an OT making $3/hour (after paying for kids’ childcare) to a full-time OT resource creator for millions of readers. Want to collaborate? Send an email to contact@theottoolbox.com.