Whether it’s the classroom, home, or day to day life…coping strategies for kids are needed. Coping strategies are mechanisms or tools to adjust and respond to emotions, stressors, and unbalance so that one can function and complete daily occupations, or everyday tasks. Coping tools help to balance and regulate a person. Coping strategies can look different for every individual and that’s why this giant list of coping skills will be powerful in building a toolbox of strategies for kids (or teens and adults!)
Coping strategies like the ones listed here can be used in conjunction with an emotions check in and feelings check in to support self awareness and self regulation skills.
the strategies that we’ve shared here are great for adding to a budget sensory room in the school environment, or a calm down corner at home.

What are Coping Strategies
We all need coping strategies! It can be difficult to cope with stress or worries as a child. Most of the time, it can be hard to just figure out what is going on with the mood swings, frustration, behaviors, and lack of focus. Most of these problems can be a result of a multitude of problems!
And, helping kids to understand the size of the problem is part of this because then we can help them know how to cope.
Self regulation strategies use coping mechanisms to support various states of emotional and behavioral levels. The Zones of Regulation and the Alert Program both use coping tools to support emotional and behavioral needs.
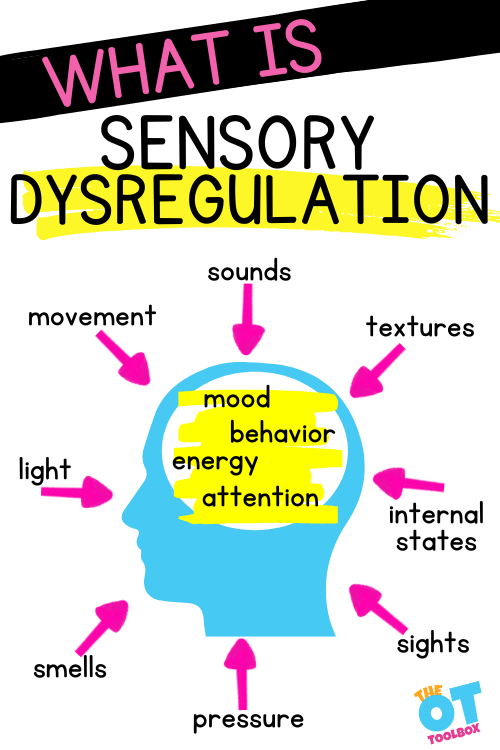
From emotional regulation concerns, to sensory processing issues, to executive functioning struggles, to anxiety, communication issues, or cognitive levels–ALL of the resulting behaviors can benefit from coping strategies.
Here on The OT Toolbox, I’ve shared sensory coping strategies for anxiety or worries. These can be used for so many other underlying concerns as well.
It’s not just anxiety or worries that causes a need for sensory-based coping strategies. Emotional regulation, an unbalanced sense of being, stress, situational or environmental issues…the list of concerns that would benefit from sensory coping tools could go on and on.
Incorporating sensory strategies and sensory play into a coping toolbox can help kids with a multitude of difficulties. Try using some of these ideas in isolation and use others in combination with one or two others. The thing about coping strategies is that one thing might help with issues one time, but not another.
Coping Strategies for Kids
One thing to remember is that every child is vastly different. What helps one child cope may not help another child in the same class or grade. Children struggle with issues and need an answer for their troubles for many different reasons. The underlying issues like auditory processing issues or low frustration tolerance are all part of the extremely complex puzzle.
Other contributions to using coping strategies include a child’s self-regulation, executive functioning skills, self-esteem, emotional regulation, and frustration tolerance. That makes sense, right? It’s all connected!
Coping Skills for Kids meet needs
Coping skills are the tools that a person can use to deal with stressful situations. Coping strategies help a us deal with occupational unbalance, so that we can be flexible and persistent in addressing those needs.
Coping skills in children can be used based on the needs of the individual child. Also, there is a lot to consider about the influence of factors that affect the person’s ability to cope with areas of difficulty. Likewise, feedback from precious coping efforts relates to the efficacy of a coping plan. (Gage, 1992).
Coping skills in kids depends on many things: wellness, self-regulation, emotional development, sensory processing, and more.
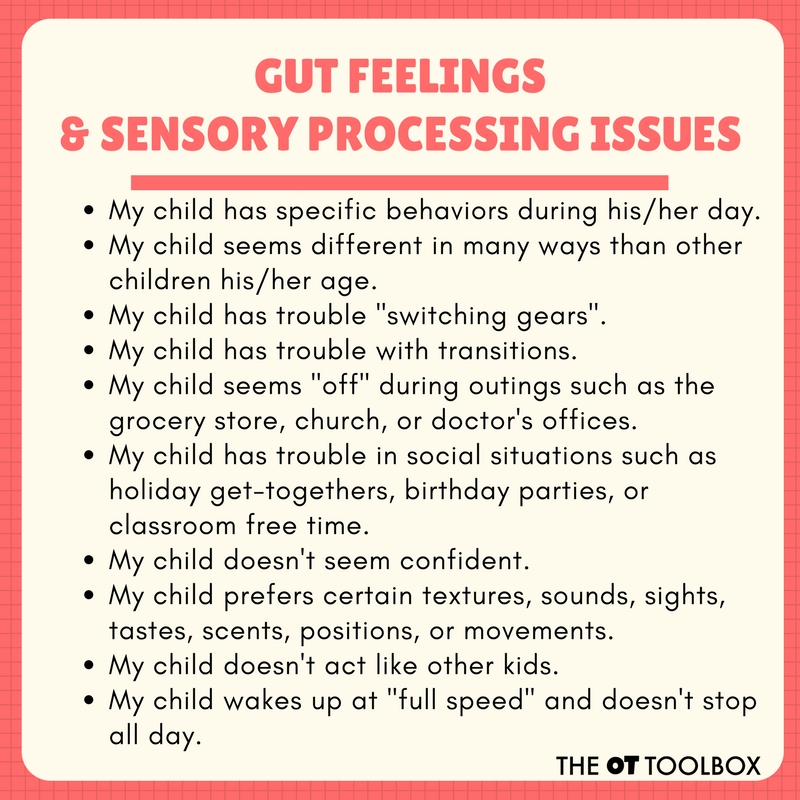
Having a set of coping skills benefit children and adults! Every one of us has stress or worries in some manner or another. Children with sensory processing issues, anxiety, or social emotional struggles know the stress of frustration to situations. It’s no surprise that some of these issues like sensory processing disorder and anxiety are linked.
Research on wellness tells us that child well being is dependent on various factors, including parental resources, parental mental health, parental relationship quality, parenting quality, father involvement, family types, and family stability. What’s more is that taking a look at the overall balance in a family and the child can provide understanding into things like stress, frustration, anxiety, and overwhelming feelings. The wellness wheel can help with getting a big picture look at various components of overall well-being.
Coping Flexibility
In fact, studies tell us that coping flexibility may be an important way to investigate coping. Coping flexibility, or an individual’s ability to modify and change coping strategies depending on the context, can be impacted by executive functioning difficulties including flexible thinking, working memory, impulse control, emotional control, and self-monitoring.
And, having more coping strategies in one’s toolbox coping may be an important precursor to coping flexibility, especially because having flexibility in coping abilities can only be obtained if an individual is able to access and use different coping strategies. It’s the chicken or the egg concept!
Another study found that children who used problem solving or constructive communication were better able to manage stress and that those who used maladaptive strategies like suppressing, avoiding or denying their feelings, had higher levels of problems related to stress. It makes sense. The most effective coping strategies are ones that adapting to the stressors rather than trying to change the stressors.
So, how can we help with stress and frustrations? One tool is having a set of sensory coping strategies available to use in these situations.
Types of coping skills
All of this said, we can break down coping skills for kids into different types of coping strategies that can be added to a coping toolbox:
Physical- exercise, movement, brain breaks, heavy work are some examples. Physical coping strategies might include pounding a pillow in frustration, using a fidget toy, running, yoga.
Sensory- While there is a physical component to sensory coping strategies (proprioception and vestibular input are just that: physical movement…and the act of participating in sensory coping strategies involves movement and physical action of the body’s sensory systems) this type of coping tool is separated for it’s uniqueness. Examples include aromatherapy, listening to music, mindfulness (interoception), and sensory play.
Sensory strategies that are motivating can be a big help for some kids. Try these train themed sensory activity ideas to get your creative juices flowing.
Emotional- Thinking about one’s feelings and emotions is the start of emotional regulation and social development. Acting out feelings, talking to a friend or teacher…communication is huge!
These social skills activities are a great way to build awareness of self and others and can double as coping tools too.
Communication- Talking about feelings, talking to others, writing in a journal, singing. Have you ever just had to “vent” your feelings about a situation? That ability to “let it all out” is a way to process a situation and talk through solutions, or find common ground in a situation.
List of Coping skills
1. Move- Get up and run in place, jog, do jumping jacks, or hop in place.
2. Fidget tools in school– Use learning-friendly fidget tools, perfect for the classroom or at-home learning space. Here is one desk fidget tool that kids can use while learning.
3. Talk- Talk about it to a friend, talk to an adult, or talk to a teacher.
4. Snuggle- Grab a big cozy blanket and pile pillows around you to build a fort of comfort! The pressure from the blanket and pillows provides proprioceptive input.
5. Take a bath or hot shower.
6. Blow bubbles. The oral sensory input is organizing.
7. Sensory water play.
8. Scream into a pillow.
9. Pound play dough. Try a heavy work dough like this DIY marshmallow proprioception dough.
10. Use a keychain fidget tool. This is a DIY fidget tool that kids can make while building fine motor skills. Attach it to a belt loop, backpack, or even shoe laces for circle time attention.
11. Exercise. This alphabet exercise activities can be helpful in coming up with exercises for kids. Use the printable sheet to spell words, the child’s name, etc. This alphabet slide deck for teletherapy uses the same letter exercises and offers exercises for each letter of the alphabet. Use it in teletherapy or face-to-face sessions or learning.
12. Look at the clouds and find shapes.
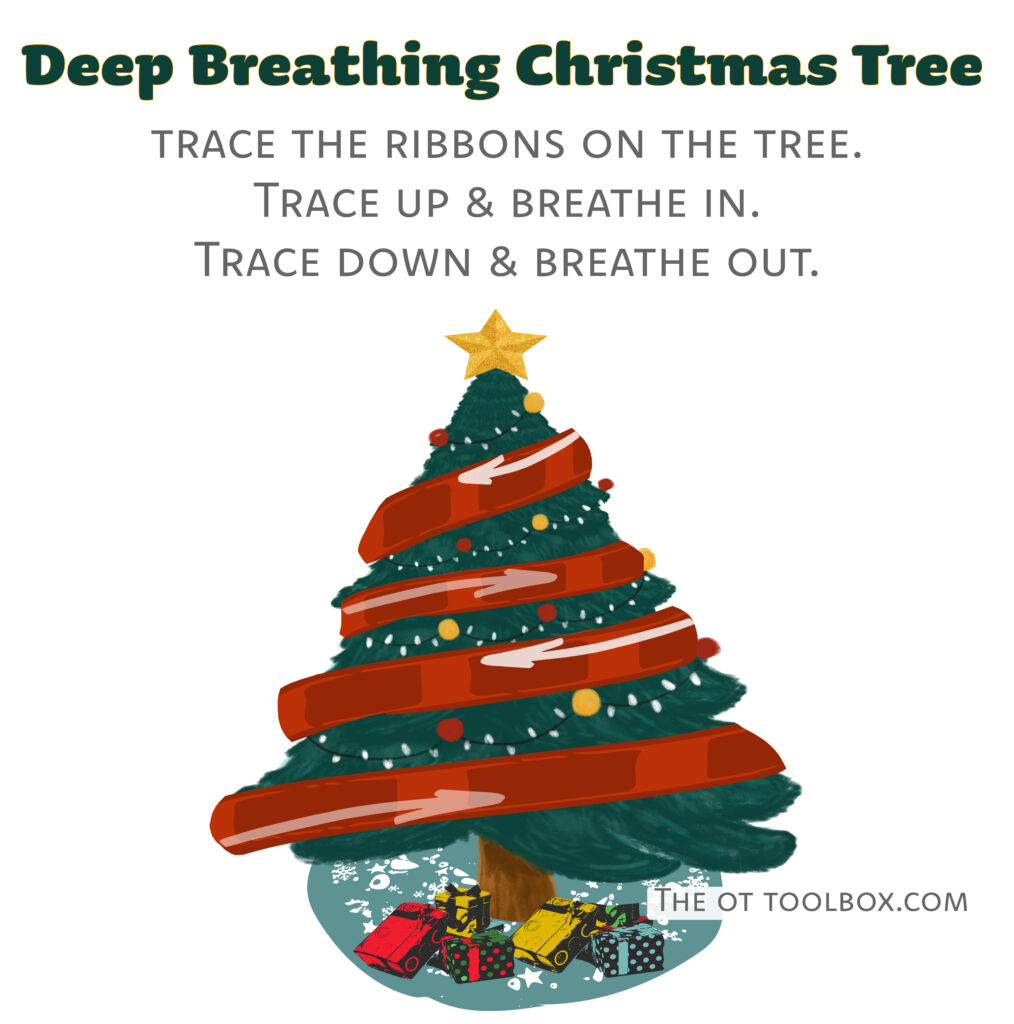
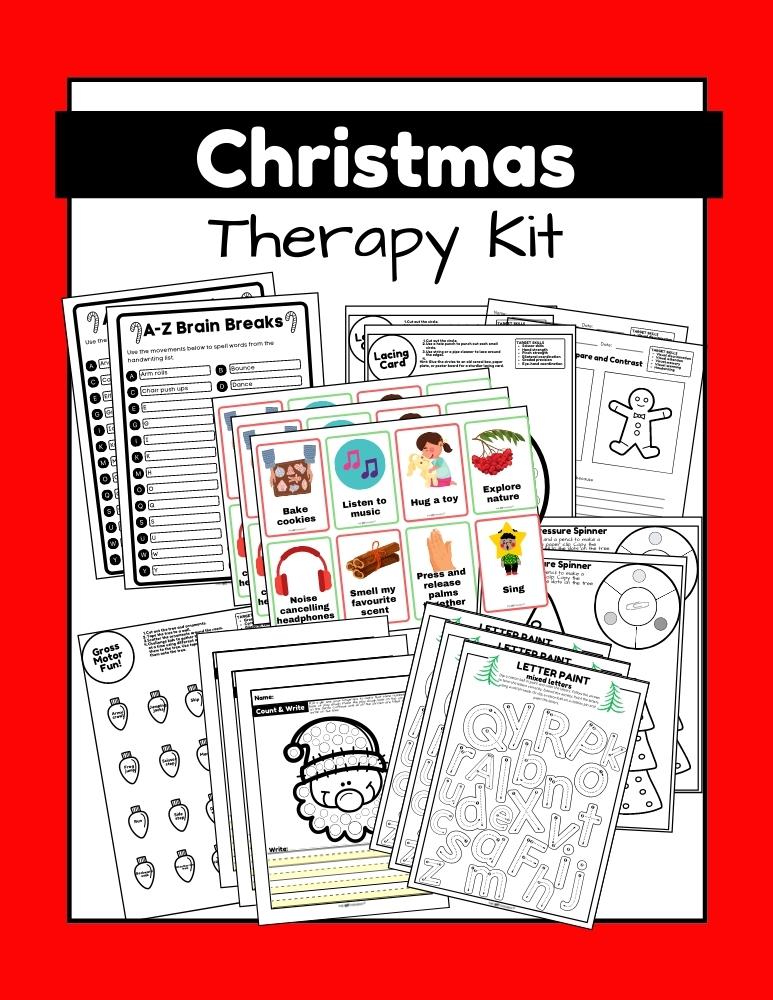
13. Deep breathing. Deep breathing exercise are a mindfulness activity for kids with benefits… Try these themed deep breathing printable sheets: pumpkin deep breathing, clover deep breathing, Thanksgiving deep breathing, and Christmas mindfulness activity.
14. Take a walk in nature.
15. Play a game.
16. Build with LEGOS.
17. Listen to the sounds of the ocean on a soothing sounds app or sound machine.
18. Count backwards. Try walking in a circle while counting or other movements such as jumping, skipping, or hopping.
19. Drink a cold drink.
20. Drink a smoothie. There are proprioceptive and oral motor benefits to drinking a smoothie through a straw. Here are rainbow smoothie recipes for each color of the rainbow.
21. Squeeze a stuffed animal.
22. Listen to music.
23. Hum a favorite song.
24. Blow bubbles.
25. Chew gum.
27. Tear paper for fine motor benefits and heavy work for the fingers and hands.
28. Smash and jump on ice cubes outdoors. Jumping on ice is a great activity for incorporating prioprioceptive sensory input.
29. Journal. The Impulse Control Journal is an excellent tool for self-awareness and coming up with a game plan that works…and then keeping track of how it all works together in daily tasks.
30. Guided imagery.
31. Think of consequences.
32. Stretch.
33. Go for a walk.
34. Write a story or draw a picture. Sometimes it helps to crumble it up and throw it away!
35. Blow up balloons and then pop them.
36. Take a time out.
37. Animal walks.
38. Imagine the best day ever.
39. Swing on swings.
40. Name 5 positive things about yourself.
41. Draw with sidewalk chalk. Drawing can relieve stress.
42. Try a pencil topper fidget tool for focus during written work.
43. Add movement- This monster movements slide deck uses a monster theme for core strength, mobility and movement breaks. It’s perfect for teletherapy and using as a coping strategy.
44. Try this easy coping strategy that only uses your hands.
45. Take a nap.
46. Sensory-based tricks and tips that help with meltdowns.
47. Use calm down toys.
HEAVY WORK coping skills
Brain breaks are a powerful and effective way to address regulation needs, help with attention, and impact learning into the classroom or at home as part of distance learning.
The impact of emotions and changes to routines can be big stressors in kids. They are struggling through the day’s activities while sometimes striving to pay attention through sensory processing issues or executive functioning needs. Brain breaks, or movement breaks can be used as part of a sensory diet or in a whole-classroom activity between classroom tasks.
This collection of 11 pages of heavy work activity cards are combined into themed cards so you can add heavy work to everyday play.
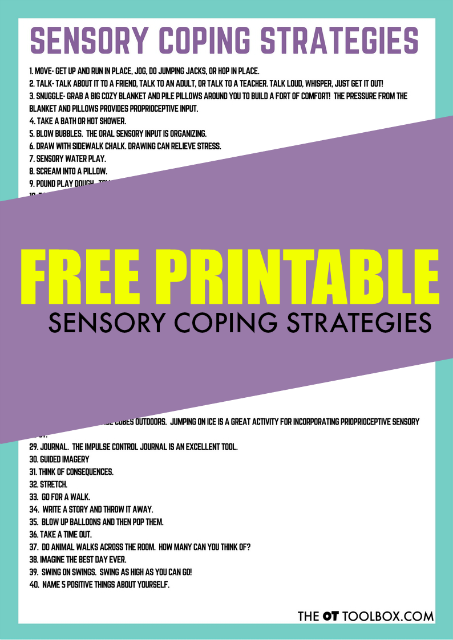
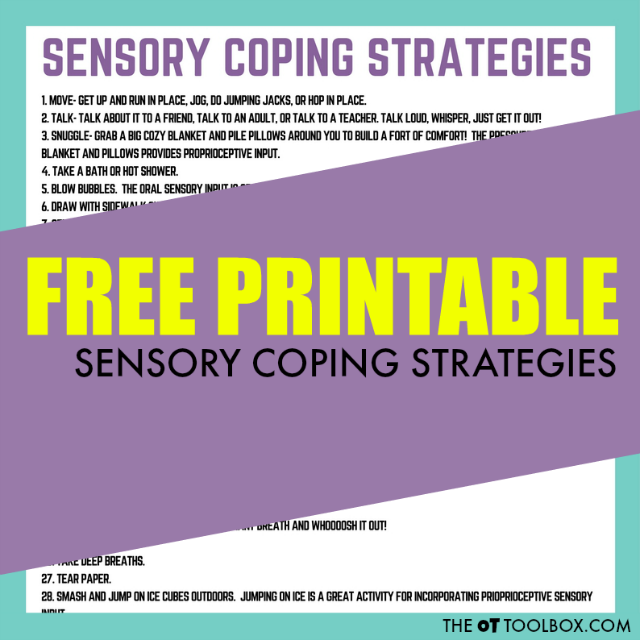
Coping strategies for kids printable
Want a printable list of coping tools for kids? This list of coping skills can be printed off and used as a checklist for building a toolbox of strategies.
Get the printable version of this list. It’s free!
Coping strategies can come in handy in many situations:
When saying “calm down” just isn’t enough…
When a child is easily “triggered” and seems to melt down at any sign of loud noises or excitement…
When you need help or a starting point to teach kids self-regulation strategies…
When you are struggling to motivate or redirect a child without causing a meltdown…
When you’re struggling to help kids explore their emotions, develop self-regulation and coping skills, manage and reflect on their emotions, identify their emotions, and more as they grow…
Gage, M. (1992). The Appraisal Model of Coping: An Assessment and Intervention Model for Occupational Therapy, American Journal of Occupational Therapy, 46, 353-362. Retrieved from : oi:10.5014/ajot.46.4.353 on 5-24-27.

Colleen Beck, OTR/L has been an occupational therapist since 2000, working in school-based, hand therapy, outpatient peds, EI, and SNF. Colleen created The OT Toolbox to inspire therapists, teachers, and parents with easy and fun tools to help children thrive. Read her story about going from an OT making $3/hour (after paying for kids’ childcare) to a full-time OT resource creator for millions of readers. Want to collaborate? Send an email to contact@theottoolbox.com.