Parents of young children may notice sensory red flags, or sensory preferences in their children that bring up a few questions. For parents of toddlers, this can be a gut feeling that milestones may be delayed, regressing, or “off”. Below, we’re covering red flags related to sensory, including toddler behavior red flags that might indicate a need for consultation with a pediatrician. Let’s go deeper…

Sensory red flags can help parents recognize their child’s’ sensory processing issues. These gut feelings can help kids to get the sensory input they need for independence and functioning.
Sensory Red Flags
Sometimes parents just know there is something “off” with their child. That deep, inner gut feeling is what lets us know that there is just something different about the way their child interacts, processes information, or performs in daily tasks.
That ability to recognize gut feelings allows us to know there is an unsuspected ear infection in our toddler or it might be the one red flag that nags at us during sleepless nights that something bigger is going on with our child.
You might have heard it said before: Mom’s always have that gut feeling about their child. Well, sometimes that inner voice can be a loud scream that a child has sensory issues or it can be a quiet nagging sense that there are underlying sensory processing problems.
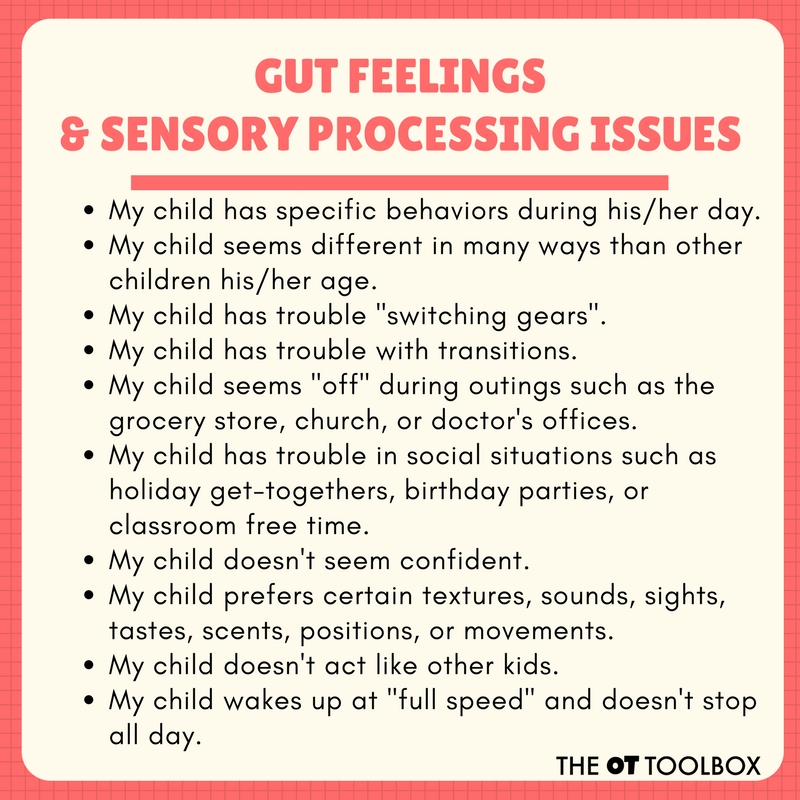
Below, you’ll find common and more unique “gut feelings” that might indicate a sensory processing problem in children. These are the quieter indications that might make you furl your eyebrows or question a behavior that your child seems to show over and over again.
Use these sensory processing red flags as a way to put the whole picture together for your child. Any one behavior or tendency that shows up with your child may be a meaningless coincidence, however if a child presents with several items on the list below, it may be necessary to speak to your child’s pediatrician.
Use these sensory processing red flags to ease that gut feeling that you have and seek out the information or help that is needed for your child.

Identifying sensory issues can mean there is a need not being meant. These sensory red flags are just some things to consider. One or two items on the list may not mean anything. Seeing many of the red flags listed below may mean that a consultation with your child’s pediatrician is in order.
Sensory Processing Red Flags
- My child has specific behaviors during his/her day.
- My child has strange tendencies.
- My child seems different in many ways than other children his/her age.
- My child has trouble “switching gears”.
- My child has trouble with transitions.
- My child seems “off” during outings such as the grocery store, church, or doctor’s offices.
- My child has trouble in social situations such as holiday get-togethers, birthday parties, or classroom free time.
- My child doesn’t seem confident.
- My child prefers certain textures, sounds, sights, tastes, scents, positions, or movements.
- My child avoids certain textures, sounds, sights, tastes, scents, positions, or movements.
- My child doesn’t act like other kids.
- My child gets upset by confined spaces.
- My child gets upset by certain sounds like lawnmowers.
- My child is difficult to calm down at times.
- My child wakes up at “full speed” and doesn’t stop all day.
- My child can not control the volume of his/her voice.
- My child can not stop jumping/spinning/bouncing/crashing.
- My child strictly avoids jumping/spinning/bouncing/crashing.
- My child is drawn to specific repetitive motions or activities.
- My child strictly avoids specific repetitive motions or activities.
- My child seems to have a problem that is difficult to pin point.
- My child seems to struggle to keep up with other kids.
- My child has no fear.
- My child has extreme fears.
- My child seems withdrawn at times.
- My child doesn’t seem to notice details.
- My child seems overly preoccupied with details.
- My child doesn’t seem to notice when they fall and get hurt.
- My child doesn’t notice dangerous situations (age-appropriately).
- My child avoids certain food textures.
Do any of these gut feelings sound familiar? There are many red flags on the list above that are conflicting signs of different problems. Not every concern that is noted above will be seen of every child with sensory processing difficulties.

Parents of toddlers are often the first to notice when something seems different or “off” with their child’s behavior. When we refer to toddler behavior, remember that we are referring to the way that the toddler acts or behaves in any given situation.
Toddler Behavior Red Flags
When therapists refer to “behavior” in the context of a toddler’s development or therapy, they are typically talking about the observable actions exhibited by the child in various daily situations. This includes how the child responds to their environment, interacts with others, and manages their emotions and impulses. There is a lot going on in toddlerhood that we can observe!
While it’s essential to remember that children develop at their own pace, there are signs that may prompt parents to seek guidance or evaluation from a healthcare professional.
Here are some common toddler behavior red flags that might be connected to sensory needs and preferences:
- Social interactions
- Fearful of others
- Little to no communication with others
- Doesn’t engage with others at all
- Won’t copy facial expressions
- Doesn’t respond to their name
- No stranger danger
- Extreme separation anxiety
- Regression in skills
- Repetitive actions like rocking, hand flapping
- Rigid patterns in play and daily activities
- Not aware of others in a room
- Limited interest in other children
- No interest in daily functional tasks such as dressing, feeding, etc.
- Fearful of stimuli
- Repetitively seeks out stimuli
- Difficulty managing certain foods or textures
- Sensitive to sensory stimuli such as lights, sounds, or textures
- Aggression
- Behind on several developmental milestones like walking, speaking words, etc.
- Delays in language or speech
- Frequent meltdowns that are out of proportion for typical toddler development
- Little to no gesture use in communicating wants or needs
- Regression in previously acquired skills such as self-care, language, or social skills
-
Self-injury
The parent questionnaire for guardians of toddlers can include some of the sensory red flags listed above, however it is geared toward the typical toddler development that happens in the 1-3 age range. This may be a time when sensory red flags become apparent to parents and guardians.
A parent questionnaire for a toddler well visit, particularly when assessing developmental milestones and potential signs of Autism, may include questions related to various aspects of a child’s behavior, self-care skills, and communication. These could be related to sensory processing needs, which impact functional performance and typical development at this age.
Here are some sample questions that could be included:
1 Communication: Some children with sensory needs may struggle with social skills and communication, which can impact their ability to understand, participate in daily activities, follow self-care instructions, etc. Communication support and social skill development may be necessary. Being aware of these milestones is important.
-
- Is your child using words to communicate their needs and desires?
- Can your child follow simple instructions, such as “give me the ball” or “come here”?
- Does your child make eye contact when interacting with others?
- How often does your child engage in babbling or attempts to speak?
2. Social Interaction: Social skills and sensory red flags go hand in hand. For more information, check out our social skills checklist.
-
-
- Does your child show interest in playing with other children or adults?
- Does your child respond to their name when called?
- Is your child able to imitate simple gestures or actions, like waving goodbye?
- How does your child react to new people or unfamiliar situations?
-
3. Behavioral Concerns: For some, activities like rocking, hand-flapping, or spinning objects may provide a calming or organizing sensory input. Noticing these behavioral habits can be a predictor of sensory needs.
-
- Are there any repetitive behaviors or unusual movements that you’ve observed in your child?
- Does your child have intense reactions to sensory stimuli (e.g., lights, sounds, textures)?
- How does your child handle transitions or changes in routine?
- Are there any specific fears or phobias that your child exhibits?
4. Self-Care Skills: Taking a look at age-appropriate self care skills in children, (or the ability to complete functional tasks like dressing, potty training, feeding, etc.) is important because at the toddler age, there should be an interest in “doing things myself” or becoming more self-sufficient. A sensory red flag may mean that there sensory sensitivities and preferences that impact the child’s ability to notice or perform age-appropriate self-care tasks independently.
-
- Is your child showing interest in self-care tasks like dressing themselves, feeding, or potty training?
- How well is your child able to use utensils and drink from a cup?
- Can your child independently perform basic self-care tasks, such as washing hands or brushing teeth?
5. Play and Imagination: Play is the work of the child but when sensory needs predominate, play can seem habitual or repetitive as a means to support sensory preferences. This can offer a sense of predictability and comfort to some children. Noticing these play preferences may convey their needs, sensory preferences, or discomfort.
-
- Does your child engage in imaginative play, such as pretending to cook, play house, or use toys to represent real-life scenarios?
- Is your child interested in a variety of toys and activities appropriate for their age?
- How does your child explore their environment and play with objects?
6. Sleep Patterns: Sleep hygiene impacts functional performance of the whole family and sometimes during the Toddler years, we see a change in these habits, possibly related to sensory needs.
-
- What is your child’s sleep routine like? How many hours does your child sleep at night?
- Does your child have difficulty falling asleep or staying asleep?
7. Feeding Habits: Sensory preferences may impact the food tolerance, resisting trying new foods, food texture issues, a tendency toward extremely picky eating, or other sensory food aversions.
-
- What is your child’s typical diet like? Are there any aversions or strong preferences?
- Is your child able to self-feed with utensils, or are they still primarily using their hands?
8. Safety Concerns- Do “sensory” considerations seem to impact direction following, the child running off in a crowded space, not listening about touching the stove or outlets, seeming to seek out unsafe situations, or other safety aspects?
-
- Are there any safety concerns or behaviors that you find challenging to manage?
- Does your child engage in any repetitive or potentially harmful behaviors?
It’s important to remember that these questions serve as a screening tool and not a diagnostic tool. If parents have concerns about their child’s development or behavior, they should discuss them with their healthcare provider for a thorough evaluation and appropriate guidance. This may be part of an indicator for exploring early intervention for Autism or other developmental needs.
Every child is different, but the concerns noted above will be indications to seek out more information and issues that should be brought up to your child’s pediatrician.
Be sure to check out our resource, our sensory processing disorder chart, to better understand how differences impact kids in different ways.
Get a free printable checklist version of our sensory red flags checklist below.

-
Fidgeting Tools for the Classroom
-
Adapted Seating Strategies for the Classroom
-
Self-Regulation in the Classroom
-
105 Calm-down Strategies for the Classroom
-
Chewing Tools for Classroom Needs
-
45 Organizing Tools for Classroom Needs
-
Indoor Recess Sensory Diet Cards
red flags checklist
Print off a copy of our Sensory Red Flags checklist. This printable tool can be a helpful resource when it comes to noticing and identifying sensory considerations that impact day to day functional performance.
To get the printable, enter your email address into the form below. You will receive a handout via email.
As always, if you suspect an area of need, consult with your child’s physician for individualized information and recommendations. This sensory red flags checklist and the toddler red flags list in this blog post is for informational and educational purposes only.
This red flags checklist is also available inside our Membership Club, along with all of the printable downloads available on The OT Toolbox website. Level 2 members can also access over 1500+ resources, sensory activities, handouts, ebooks, and much more.

Colleen Beck, OTR/L has been an occupational therapist since 2000, working in school-based, hand therapy, outpatient peds, EI, and SNF. Colleen created The OT Toolbox to inspire therapists, teachers, and parents with easy and fun tools to help children thrive. Read her story about going from an OT making $3/hour (after paying for kids’ childcare) to a full-time OT resource creator for millions of readers. Want to collaborate? Send an email to contact@theottoolbox.com.
For more information on sensory processing, development, and how to incorporate sensory needs and preferences into daily life, check out our ebook, The Sensory Lifestyle Handbook.
The Sensory Lifestyle Handbook walks you through sensory processing information, each step of creating a meaningful and motivating sensory diet, that is guided by the individual’s personal interests and preferences.
The Sensory Lifestyle Handbook is not just about creating a sensory diet to meet sensory processing needs. This handbook is your key to creating an active and thriving lifestyle based on a deep understanding of sensory processing.