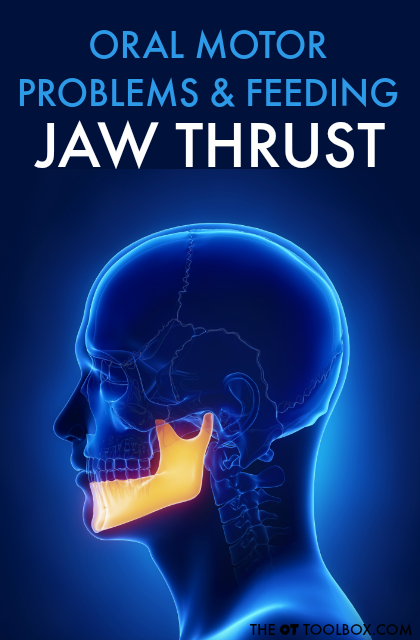
You might be following along with our series related to oral motor problems that relate to feeding. In it, we are covering all of the specifics about oral motor problems that translate to difficulty with eating and drinking. So far, we’ve covered jaw thrust but have more oral motor problems that will be covered in the coming days. Today, exaggerated jaw movements are addressed, along with the cause of these movements and how they relate to feeding issues.
Start by reading more about development of oral motor skills.
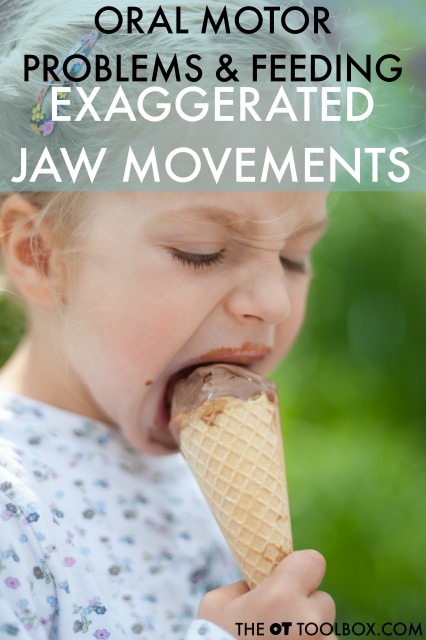
Exaggerated Jaw Movements Oral Motor Problems
Exaggerated jaw movements are different from jaw thrust in that the movements are not forceful. When exaggerated jaw closure occurs, it can be a compensation strategy for jaw instability or
There are several reasons for these exaggerated jaw movements:
Fluctuations in muscle tone
Impaired oral control
Decreased muscle tone
Exaggerated excursions can be an overflow or organizing movement
Increased oral tone
Oral hypersensitivity to the teeth touching teeth, utensils, tongue, food, straw, or a drinking cup
Poor sustained jaw closing
Jaw instability
Poor graded movement patterns
Feeding issues related to exaggerated jaw movements:
Exaggerated jaw movements interfere with stability needed for drinking from a straw, cup, or bottle, removing food from a spoon, biting, or chewing.
Stability in the jaw is necessary for efficient swallowing and controlled eating.
When the jaw’s movement patterns are exaggerated, an individual spills food and is at risk for aspiration due to difficulty with swallowing.
Graded movements on a cup or utensil are difficult, resulting in food spillage or drooling.
Oral Motor Exercises for the Jaw
If you are looking for exercises related to common oral motor problems, this FREE printable pack of oral motor exercises goes along perfectly with the series I have planned for you. Get your free printable packet of 20 different feeding therapy ideas AND 20 oral motor exercises. These are treatment ideas for oral motor problems that professionals can utilize over and over again.