Many times, OT professionals receive referrals for oral motor problems and feeding. It’s through oral motor occupational therapy interventions that kids can move from challenges biting, chewing, and moving food around inside the mouth, to success with eating and trying new foods. Let’s get started!
Oral motor problems lead to difficulty biting, chewing, and manipulating foods. They can cause difficulties with textures of foods, and can be a cause of extremely picky eating! A good place to start is with understanding the development of oral motor skills.
Oral Motor problems
One thing is for sure; individuals can have a huge spectrum of considerations when it comes to oral motor issues. No two kiddos will be alike. That’s why it’s so important to discuss oral motor issues with a professional.
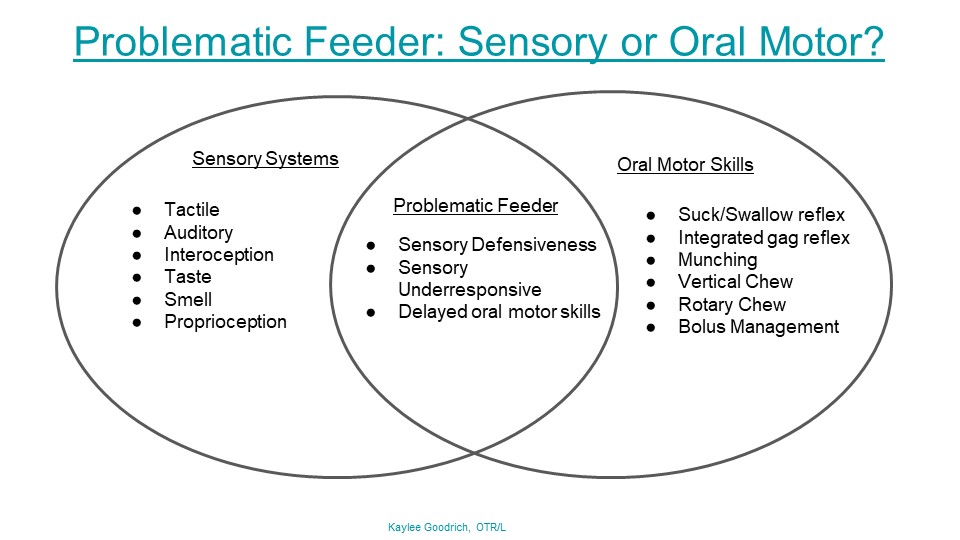
The process of eating is a complex collection of movements patterns with physical and sensory components.
When feeding is a challenge, many times individual oral structures and sensory-motor patterns are a cause.
If you are questioning whether an eating issue is sensory or oral motor, be sure to take time to explore each consideration. There can be different interventions and strategies depending on the underlying cause of eating difficulties. For example, there are specifics when it comes to issues with sensory food aversions and sensory food issues.
What are Oral Motor Problems Occupational Therapy Addresses?
The oral motor problems listed below are just some of the issues that can impact function in feeding.
In a small series of blog posts, I have broken down each oral motor problem that occupational therapists typically address. Each blog post includes information about the specific oral motor concern, the reasoning or underlying influences that relate to each oral motor issue, and feeding issues related to the specific oral motor problem.
This series of blog posts should be a resource for you to find more information relating to how feeding issues are related to specific oral motor problems and how these feeding issues can be addressed in treatment.
Click on the links below for more information on each oral motor problem area as they relate to feeding.
- Mouth Clamped Shut when eating- Consider the child who clamps their mouth shut during meals. This is usually the biggest sign to a parent that the child is all done eating, is full, or is refusing to eat. However, it might be an oral motor problem that is actually the cause of the clamped shut mouth. The child falls back on this technique because it’s worked for them in the past in some way to provide stability, move out of the difficult oral motor exercises, or has resulted in a response from the parent.
Other oral motor problems include:
- Tooth Grinding
- Tonic Bite
- Jaw Retraction
- Tongue Retraction
- Tongue Protrusion
- Tongue Thrust
Occupational Therapy for Oral Motor
Oral motor interventions in occupational therapy can cover a variety of intervention techniques. It is essential to begin with an evaluation and individualized assessment by a feeding professional. Occupational therapists are trained in this area, but some OTs have additional certifications.
The list of occupational therapy oral motor strategies listed below is for educational purposes only and not a replacement for therapy of any kind.
Some occupational therapy oral motor strategies that can be used are:
- Oral motor assessment- It is essential to start with the assessment process for safety of the individual. Addressed in more detail below.
- Oral motor stimulation- In occupational therapy, strategies include brushing to the lips or cheeks, towel stimulation, feeding swab, tongue mobility exercises, etc. These are explained in greater detail below.
- Oral Motor Exercises– We’ve listed a larger list of specific exercises to use in play and in therapy sessions.
- Oral motor coordination exercises– Use the oral motor cards in the deep breathing kit to improve oral motor coordination skills. Try mimicking the movements by using a mirror and visual modeling.
Oral Motor Assessment Occupational Therapy
Assessment occurs by a pediatric occupational therapist, but there are many things to be considered.
Feeding is developmental and it’s essential to consider the level, age, and abilities of the individual as this will impact all aspects of feeding and oral motor considerations.
Oral motor assessment and infants-
In infancy, oral motor skills are both a means for self-regulation (nurturing through sucking) and nutritive. Things to consider in an occupational therapy oral motor assessment for infants and babies at this age and stage:
- Is the infant able to suck in exploration for nipple of bottle or breast?
- Does the infant suck in bursts and have pauses to allow for breathing while eating?
- Assessment of the physical mechanics of swallow
- Timing of sucking and pauses- sucking should occur at a rate of about one suck per second with pausing to swallow the liquid and breathing. This should occur in a coordinated manner.
- Lip closure
- Jaw movements to draw liquid into the mouth and to swallow (infants)
- Anterior tongue movement during the sucking, along with cheek movement and jaw movement as the tongue draws milk or formula to the rear of the mouth to swallow (older babies)
- Oral reflexes and whole body primitive reflexes (root reflex, a suck reflex, a swallow reflex and then protective reflexes like gag and coughing)
- Liquid leaking from the mouth during eating
- Anatomy of the mouth, tongue, lips, neck, etc.
- Positioning during feeding
- Family educational needs
- Sleep and timing considerations
Oral motor assessment in babies–
In older babies, you begin to see certain developments. Missing these milestones can indicate oral motor problems. These considerations should be addressed in occupational therapy oral motor assessments as babies grow:
- Hands in the mouth in exploration and play- this is normal part of exploration and supports development of tongue, lips, cheek mobility
- Positioning and seating (high chair positioning)
- Neck, head, and upper body control against gravity
- Motor coordination at age appropriate levels
- Bite reflex
- Mouthing toys, teethers, etc.
- Making sounds with a variety of oral motor movements
- Mimic facial expressions (open mouth, tongue out, etc.)
- Gag reflex present
- Accepting variety of baby food textures, flavors
- Accepts foods from a baby spoon
- Lip closure
- Tongue mobility (thrusting tongue after initial spoon offerings is normal)
- Transverse tongue reflex- The baby/child feels stimulation on the side that tongue and the tongue moves in that lateral direction- needed for swiping foods
- Attempts or tries a variety of flavors, textures, and softer, larger foods
Oral motor assessment in toddlers-
During the toddler years, oral motor issues can present in drinking, feeding, and other areas. Consider these aspects in OT assessments:
- Drinking from sippy cup/open cup
- Drinking from a straw
- Drinking a variety of textures and thicknesses (water, juice, thick or thin smoothies
- Eating a variety of textures and thicknesses
- Eating fluids mixed with solids (cereal, soups)
- Biting foods from a larger piece of food
- Moving food around within the mouth
- Swiping the mouth with the tongue to clear the mouth
- Chewing with rotational movements of the jaw
- Begins to remove food from the lips with the tongue
Oral motor stimulation
We cover specific oral motor exercises designed to support the oral motor stimulation to move the lips, tongue, and jaw to bite, move, swipe, clear the mouth of food, and swallow food in our resource on oral motor exercises. However, below you will find strategies to provide oral motor stimulation to the mouth, lips, gums, and tongue.
Oral motor stimulation in occupational therapy centers around play in order to enable function. This focuses on independence with feeding with safe ability to bite food, clear food from the mouth with the tongue so that food can be swallowed.
Tongue Stimulation-
- Use a mouth swab– to touch, swipe, tap and swab the tongue on the sides, at the tip, and along the length, avoiding the back of the tongue to avoid activating a gag reflex.
- Use a vibrating toothbrush- to stimulate tongue movement on the sides. This can help the tongue with lateral movements.
- Use a gloved finger- Put on a latex or non-latex glove and use a finger to tap the sides of the tongue. The glove can be worn by either the occupational therapist or the individual themselves.
- Use a mirror- Move the tongue by mimicking movements and watching them in a mirror. You can even have the individual touch their tongue to a clean mirror surface. Play in front of a mirror alongside the child or in front of the child above the mirror so the child can look at the therapist’s face and check their movements in the mirror at the same time.
- Tongue movement exercises- Use the tongue and mouth exercises included in our Deep Breathing Exercise pack for ideas.
- Tongue sounds- Make clicking sounds with the tongue on the roof of the mouth. As the child/individual to copy the sounds.
- Push the tongue into the cheeks of the mouth to copy motions. This can help with lateral sweep of the tongue to clear foods by increasing tongue range of motion.
Lip and Cheek Stimulation–
- Washcloth oral motor simulation- this occurs with a dry wash cloth and then a wet wash cloth by rubbing the lips and cheeks. Each area can be separated so they are addressed in isolation. Use a dry washcloth or wet washcloth to wipe the face, without food use. Use a warm or cold washcloth to wipe the face.
- Making faces- Cheeks and lips can obtain heavy work, or proprioception by puffing up the cheeks, making fish lips, sealing the lips and blowing, blowing raspberries, copying facial expressions, etc. Play “Simon Says” with facial expressions. We have oral motor Simon Says Commands to share!
- Food stimulation- Some foods (sweet, sour) are very alerting. These can be used as a frozen pop in the form of a lemonade pop, smoothie, or popsicle. Or, add fruits and frozen foods to a mesh bag that is sucked on.
- Ice pops- Freeze an ice cube on a popsicle stick and use it as an alerting and stimulating tool to “wake up” the lips and cheeks.
- Vibrating tools- Play with vibrating mouth toys and touch the face, mouth, lips, teeth in the way of a vibrating toothbrush (offering input through the jaw).
- Wilbarger Brushing Protocol– Use prior to eating foods (contact a trained therapy professional)
Jaw Stimulation-
- Vibrating toys- vibrating toys, chewing tools, or a vibrating toothbrush can offer oral motor stimulation through the jaw. This can be very alerting, so use with caution.
- Chewing tools- biting on “chew toys” (described as heavy chewing therapy tools) or chewing tools that add heavy work through the teeth and jaws. This offers feedback to “wake up” the jaws.
As you can see there is a lot of different areas that need to be assessed and addressed when it comes to oral motor concerns related to eating and drinking.

Colleen Beck, OTR/L has been an occupational therapist since 2000, working in school-based, hand therapy, outpatient peds, EI, and SNF. Colleen created The OT Toolbox to inspire therapists, teachers, and parents with easy and fun tools to help children thrive. Read her story about going from an OT making $3/hour (after paying for kids’ childcare) to a full-time OT resource creator for millions of readers. Want to collaborate? Send an email to contact@theottoolbox.com.



 A little about Kaylee:
A little about Kaylee: