Teaching a child how to hold a spoon and scoop food requires several motor skills that must be developed before a toddler can use utensils themselves. Even older children struggle with the ADLs of holding a spoon and scooping food to feed themselves. Here, we’re covering sensory motor skills needed to hold a spoon, fork, knife, and other utensils. You’ll also find some creative activities and play ideas to develop the underlying skills that play into using utensils.

Note that these strategies and skill areas are needed across the lifespan when it comes to self-feeding. Older children and even adults who may have had a physical or cognitive impairment can benefit from addressing the underlying skill areas needed for using utensils. No matter the age, noting how an individual holds a spoon and fork is part of a comprehensive feeding evaluation.
how to hold spoon and fork
Before we get to the skills in play when holding a spoon or using a fork, let’s cover the specifics on how to hold these utensils. Why? Because often, we see older children who hold a spoon with a gross grasp or hold a fork with the whole hand. These grasp patterns can impact functional performance, but can also be a cause of concern for parents.
Note that the way an individual holds a spoon or holds a fork can differ when adaptive equipment for eating is used.
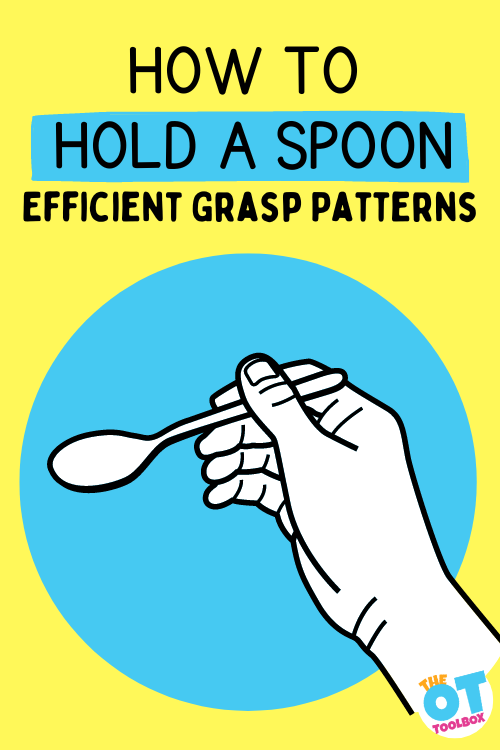
how to hold a spoon
To hold a spoon, one needs to grasp the utensil with their dominant hand.
- The spoon is placed along the lateral edge of the middle finger or pad of the middle finger.
- The pointer or index finger typically rests over the top of the neck of the spoon, and guides movements when scooping.
- The thumb rests and stabilizes the flat handle of the spoon on the top, above the pointer finger in a modified lateral key grasp.
- The scoop of the spoon is pointing out toward the direction the thumb points, and the handle is above the thumb web space.
In this position, one can scoop with refined movements and graded precision using the pad of the thumb on the flat part of the spoon handle. When the spoon is properly placed in the hand, the wrist is slightly pronated and slightly flexed.
You can see from the image below that there are many different grasp patterns used when holding a spoon, which progress as the child develops more refined fine motor skills. The most efficient grasp pattern is the “adult grip”, however, the other grasp patterns are typically part of a progression as the toddler or young child gains experience with eating with a spoon.
Using a spoon is likely one of the first functional tools that a small child has experience with, and while messy eating will ensue, it is important to allow the baby or toddler experience with holding and manipulating a spoon, even if they are not getting actual food into their mouth at first.
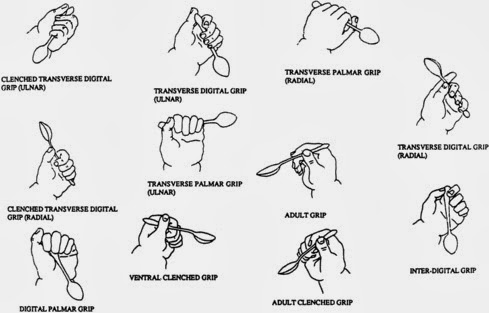
No source was found for this image, may be subject to copyright
Inefficient grasp on a spoon- When the handle end of the spoon is UNDER the thumb web space, the grasp moves into a poor position for function and accuracy of scooping. In this case, the hand moves into a gross grasp pattern, and in order to gain motor control with graded precision, the elbow tends to pop out as the shoulder abducts. In this poor functional grasp pattern, you’ll see the wrist fully supinated.
Activities to move from an inefficient grasp pattern to an efficient grasp pattern include PLAY:
- LightBrite activities
- Play dough
- Blocks
- LEGO
- Building toys
- Hand strengthening activities
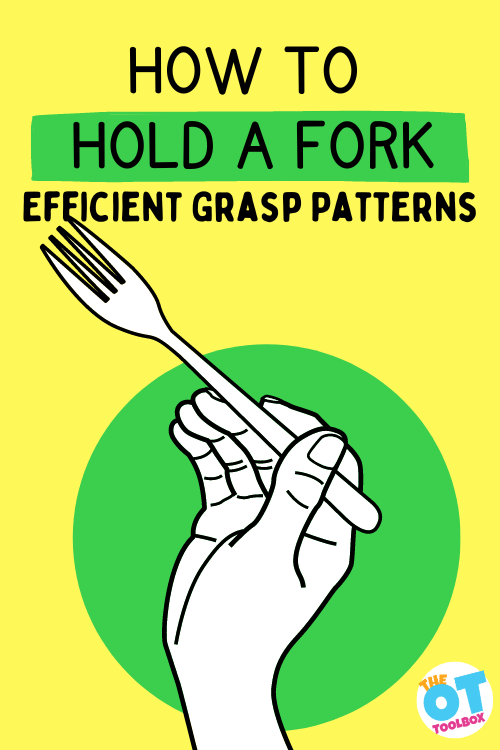
how to hold a fork
Next, let’s cover the proper grasp pattern required to effectively hold a fork. Note that there are different ways to hold a fork, depending on location, no one way of these different style being better or worse for functional performance to hold and use a fork to stab and eat food.
To hold a fork, the fork is held in the dominant hand much like a pencil is held. The thumb stabilizes the narrow part of the fork handle, or the neck of the fork. This area is located above the prongs, or tines of the fork. The neck of the fork rests on the lateral side of the middle finger or the pad of the middle finger.
Like holding a spoon, the end of the fork is above the back of the hand, and not under the thumb web space into the palm.
The wrist of the hand should be slightly pronated and slightly flexed.
Note that when holding a fork to scoop food, a different grasp pattern is used than when using a fork to stab food, and still another grasp pattern is used to stabilize food when using a knife to cut.
To stab food with a fork, the fork rotates in the hand and skills of in-hand manipulation are used.
To stabilize food with a fork, in order to hold food stabile so a knife can cut the food item, the fork continues to rotate within the hand using in-hand manipulation, but the addition of finger isolation of the index finger is used to hold the fork steady.
Inefficient grasp on a fork– When the end of the fork handle is under the palm, the hand tends to pull into a gross grasp on the fork, which is a more primitive grasp pattern, and is less functional for refined and graded movements. Similar to the motions used with a spoon held in this manner, a fork held in a gross grasp will include elbow and shoulder.
Much like using a spoon, progression from inefficient grasp patterns on a fork is developmental and requires practice. Allowing kids to use and hold a fork with verbal and visual prompts is helpful. Other fine motor and eye-hand coordination tasks will support development from inefficient grasp patterns when holding a fork to more efficient and refined motor skills:
- Playing with play dough and using play dough tools like play knives, play forks, and sculpting tools
- Cutting with scissors
- Finger isolation activities
- Dropping items like cut straws or pipe cleaner pieces into a bottle
- Sorting coins into a piggy bank or recycled containers with slotted lids
- In-hand manipulation activities
We’ve created a video that shows how different grasp patterns impact functional use in holding and using a spoon and fork. If you can’t view this video, we’ve also posted the activity ideas to help kids hold a spoon on our YouTube channel.
Prerequisites to hold a spoon and fork
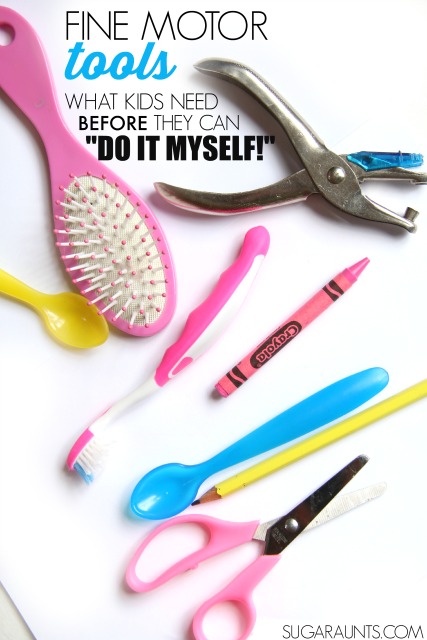
Before a child can use fine motor tools such as a spoon, fork, knife and other self-care tools (hair brush, toothbrush, pencil, scissors…) independently, there are certain physical, cognitive, and emotional prerequisites that must fall into place.
These self-care skills include many of the same sensory motor components, so in this blog post, we’re covering primarily the skills needed to hold a spoon and fork.
Toddlers and young preschoolers that sit at the table, probably have taken notice of how adults and older children at the table eat. This is actually part of the developmental process. When sitting at a table, a baby and toddler is observing and noticing how older siblings and parents use forks to stab food, spoons to scoop, and knives to cut.
Toddlers often want to take part in the action!
Using a spoon and fork during the Toddler years is a natural development of self-awareness and self-control. Using utensils is part of that progression of feeding developmental milestones that children go through. A child becomes more aware of the skills that they are developing and that they can assert their own independence.
Likewise, using a spoon to eat at first can lead to messy eating with young children, and that’s totally normally, developmentally.
But, before these areas of independence arise, there are certain prerequisites that need to be in place. Using tools in self-feeding, brushing one’s own teeth, using a knife, crayon, pencil, or other tool requires development in a few areas.
Speaking of using crayons to develop motor skills, these crayons for toddlers support fine motor development and coordination skills through play.
This post contains affiliate links.
Skills Needed to Hold a spoon and fork
When you take a look at the motor breakdown of using a spoon and fork, there are several components you’ll see in action:
- Posture
- Grasp Development
- Hand Preference
- Cognition
- Attention
- Eye-hand coordination
- Somatosensory experience
- And even play!
Let’s cover each of these areas needed to hold a spoon and fork in more detail:
- Posture- When using a tool like a fork, pencil, scissors, toothbrush, paint brush, knife…postural control is essential. Like anything else, it all starts at the center and at the body. You can’s use your hands in fine motor play activities if your upper body is slumped or slouched. If postural support is the issue, work on getting into a better sitting position. Speak to an Occupational Therapist for individualized assessment and recommendations.
- Grasp Development- For using tools, a child needs prehension skills and precision skills, including grasp, release, and the ability to stabilize their arm and write while moving the hand. Sometimes a pinch or required muscle movement is too much for an unstable arm/wrist and that required muscle effort makes the upper body slouch. Start over with posturing is this happens.
- Hand dominance– A true hand dominance doesn’t typically become established until 5-6 years. And that is a good thing! A child’s body is developing strength, balance, muscle tone, and sensorimotor abilities at an even and symmetrical rate in the early years. We want that to happen! If a very strong preference of dominance is noticed at an early age, ask your pediatrician or occupational therapist for assessment of asymmetry or delay.
- Cognitive prerequisites– Appropriate ability to follow simple directions is a must in order for use of tools in typical ways. Sure, a fork makes a great hair brush. A spoon is an excellent drumstick. But, inappropriate use of utensils can be dangerous.
- Attentional Prerequisites– Appropriate attention span is needed for using tools in functional tasks. This blog post covers more on attention needed during meals.
- Constructive play– What? A child needs functional play in order to use a pencil? Yep! Building with blocks, combining toys, and pretending provides the base of fine motor development, skilled use, strength, imagination, and creativity that is needed to problem solve and use tools appropriately.
- Eye Hand Coordination– More play! Catch a ball and use crayons to establish the base of hand eye coordination needed for skilled maneuvering of tools to the mouth, paper, hair, or teeth.
- Somatosensory Experience– Playing and experiencing the senses in typical every day activities are essential for the child to build on their awareness of textures, weights, manipulating objects, and sizes.
Given all of these areas that a child must have in place before showing success with tools in functional tasks, it’s important to work on certain areas.
Below, you’ll find a great printable resource that covers all of these skill areas that are needed for using a spoon and fork. This is a great handout to use especially when working with families of young children who are learning to hold a spoon and fork.
You can enter your email address into the form below and access this printable handout, or The OT Toolbox Member’s Club members can log into their accounts and access the handout in the Educational Handouts Toolbox area.
Scooping food with a spoon
Teaching kids how to hold a spoon is the first step, but then actually scooping food, getting the food to the mouth, clearing the food from the spoon, and then repeating the process is part of the functional task of eating.
Remember that eating is a developmental process, and that this is another occupation in which practice is key to functional performance!
To improve use with a spoon and fork (and then spoon, fork, and knife!), it’s important to have various opportunities for practice.
Provide opportunities to use tools like spoons in scooping items. You’ll find more information on the topic of scooping in our blog post on scooping and pouring.
These black beans are a great way to practice tool use and all of the skills needed in managing tools. See the bottom of this post for more ideas.
Be sure to provide your little one with lots of opportunities to use tools in activities and play!
Related activities that you will love for teaching kids to use tools:
- Sight Word Scoop– this scooping activity encourages users to develop the eye-hand coordination needed to use a spoon to scoop an object in a liquid, much like scooping the remaining cereals in a bowl of milk, or scooping food from a soup broth.
- Toddler Visual Motor Scoop (Ping Pong balls)– This activity is another great way to teach toddlers to use a spoon, using a large and bright object with high visual contrast.
- Invitation to Scoop and Pour– In this activity users can use a spoon with graded precision and refined movements to scoop grains of corn which can be a great way to practice motor skills to hold a spoon.
- Field Corn Sensory Bin– Another activity using spoons to scoop field corn, this activity offers proprioceptive feedback through the joints and muscles of the hand, wrist, elbow, and shoulder.
- Moon Dough Scooping– In this activity, users use a spoon to scoop and pick up a moist and dry material. This can be a great way to practice using a spoon with different materials.
- Scooping Ice– Using a spoon to pick up ice is a fun way to practice using a spoon with a different material that also offers precision and refinement in using a spoon or scoop.
- Relaxing Lavender Water Bin– Kids love this sensory bin, but therapists love the functionality! Use a spoon to pick up small items in a liquid, developing eye-hand coordination skills with sensory benefits.
- Invitation to Scoop, Pour, Transfer Nuts– Use a spoon to pick up nuts with a fun sensory activity that offers feedback with movement.
- Scooping Dyed Alphabet pasta– Kids can pick up dry pasta with a spoon and practice motor skills.
- (Amazon affiliate link) Learning Resources Handy Scoopers are colorful and bright and a great way to practice the prerequisites for tool use in many ways.
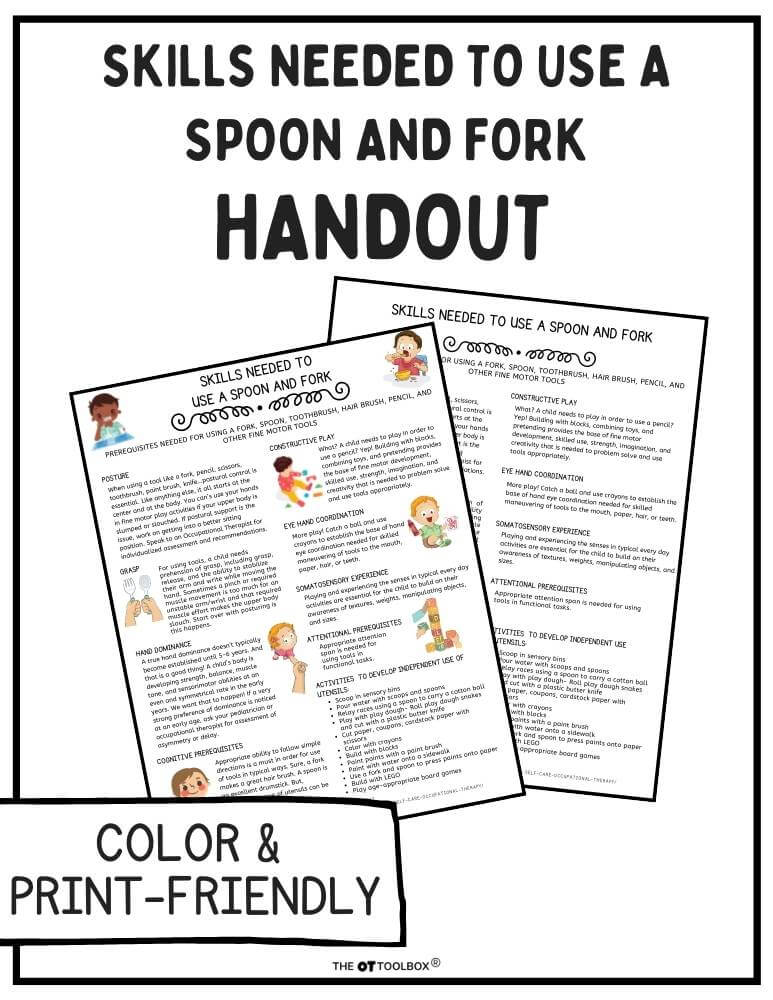
Free Handout- Skills Needed to Hold a Spoon and Fork
Want a printable handout of the skills kids need to hold a spoon and fork? Working with families on teaching kids how to hold a fork and spoon and need actionable tips and strategies in a handout format?
You can enter your email address into the form below and access this printable handout, or The OT Toolbox Member’s Club members can log into their accounts and access the handout in the Educational Handouts Toolbox area.

Colleen Beck, OTR/L has been an occupational therapist since 2000, working in school-based, hand therapy, outpatient peds, EI, and SNF. Colleen created The OT Toolbox to inspire therapists, teachers, and parents with easy and fun tools to help children thrive. Read her story about going from an OT making $3/hour (after paying for kids’ childcare) to a full-time OT resource creator for millions of readers. Want to collaborate? Send an email to contact@theottoolbox.com.