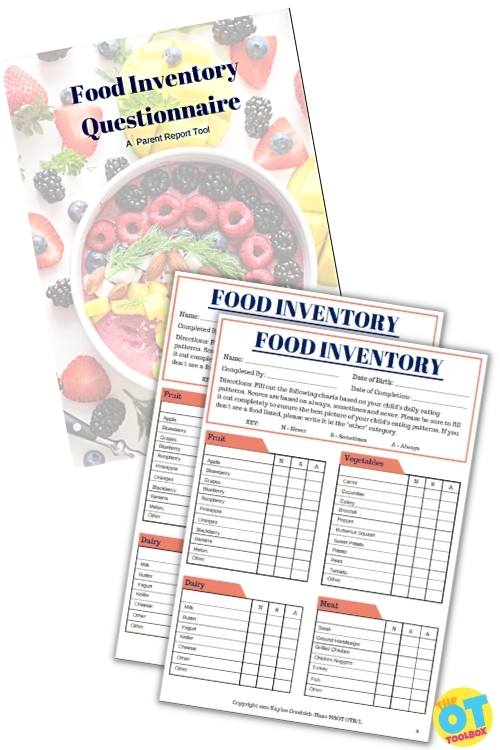
An integral part of an occupational therapy feeding evaluation is the food questionnaire or checklist. This is the foundation for building your learner’s food repertoire based on their likes and dislikes. When discussing preferences with the parent and child, the more details they are able to provide, the smoother the sessions will go.
How to Do a Feeding Evaluation
The first step to a feeding evaluation is often a comprehensive Food Inventory Questionnaire. By understanding what a child is and is not eating helps the therapist to better understand food preferences in the way of food texture issues, flavors, colors, tec.
The food inventory is a great tool for consistent data collection. Accurate data collection will helpful be able to provide a just right challenge. Before beginning any feeding program, it is important to become educated on feeding therapy, treatment, and problem areas in a thorough feeding assessment. This guide will provide a basic understanding of sensory versus oral motor feeding concerns.
Check out the tips below to help guide your discussion.
When Planning a Feeding Evaluation, Provide Questionnaires Ahead of Time
The first tip we as OTs love to recommend refers to the pre-referral information. It’s so helpful to get that background information ahead of time.
If at all possible, try to provide a feeding assessment checklist or questionnaire ahead of time, or ask the parent to come prepared with a list of foods that their child does or does not like. This is SUPER important, because asking a parent during the feeding evaluation, does not typically go well.
It is likely that you will not get a complete picture, or the parent will forget some key pieces of information–such as what brand of cereal their child eats or be so overwhelmed they claim their child eats “nothing”.
Not all of the problems presented will be sensory food issue related. There are times when they stem from an oral motor deficiency. It is important to be able to spot the difference before beginning treatment.
During a Feeding Evaluation: Ask About Food Jags
Tip number 2 when it comes to feeding evals refers to food jags. As parents, you’ll want to tell your therapist about these! And evaluating therapists: make sure you ask if food jags are present.
What is a Food Jag?
The term “food jag” is fairly new term referring to a preference toward a couple of foods, eating them all of the time; suddenly stopping eating a once highly preferred food, refusing to add it back into their repertoire. A food jag refers to the case of children only eating one type of food or a small number of food items. Some common food jags include:
- The child that only eats chicken nuggets, crackers, and French fries (all foods are consistent in taste and texture.
- The child that only eats Goldfish crackers, dry cereal, and crackers (all foods are bland, have some crunch, but are thin in width
- The child only eats yogurt tubes or yogurt smoothie drinks (the consistency and sweetness of the yogurt flavors are satisfying)
Food jags include any small group of limited food selections. These food limitations can change over time.
You’re looking to see if this has happened over the course of the child’s feeding history as it may be indicative of trauma (i.e.-choking), emergence of sensory processing difficulties, and feeding developmental milestones that occur in leaps and stages.
This is also common in people who do not eat a variety of foods. They get tired of eating the same three foods over and over. Food jags can happen to people who eat a variety of foods also, but generally people have other foods to put in its place.
For instance, I may eat peanut butter and jelly sandwich every day for three weeks, then get tired of it. That is fine because I can switch to yogurt, or ham, or turkey. A person with limited food choices loses a preferred food and does not have anything to replace it with.
If you notice a trend of food jags in the child’s history, make sure that you provide education on how food jags occur and how to prevent food them, before they leave the evaluation.
Complete a Sensory Evaluation of Food- Review Each Food Category
Tip number 3 for a comprehensive feeding evaluation refers to the sensory aspect of feeding. We really want to break down various foods by category and consider the sensory contributions of the different types of food. Considering how different food is based on sensory factors can open doors for offering new foods in therapy interventions. Just explaining that to parents can turn on a lightbulb!
Even if the parent fills out a feeding assessment checklist/questionnaire and hits all the food categories, fruits, vegetables, starches, dairy, protein (meat, eggs, nuts) and other (snack foods), make sure that you go through the list with the family.
When you review each category, even briefly, it may spark the parent to remember something regarding the child’s eating patterns.
Consider the sensory evaluation of food including differences in types of food categories, and how there can be minute or vast sensory differences in foods based on preparation (cooked in the oven or cooked in the microwave, different brands (drier consistency vs. saltier flavor), or types of foods (spaghetti pasta vs. smaller elbow noodles).
A food evaluation should take the sensory evaluation of foods into consideration for each meal.
Questions to ask regarding food preferences:
For example, if the parent reports that their child eats noodles, you might want to ask what kind of noodles.
- Do they eat only elbow noodles?
- All types of noodles?
- And all varieties of noodles-egg noodles, veggie noodles, rice noodles?
Another example of food variables is seen in fruit.
- Fruit can be whole, peeled, fresh or comes in a container.
- Apples can be peeled, sliced, or presented whole.
- How does the child eat them?
- Mandarin oranges come in syrup or can be freshly peeled. Which does your learner prefer?
If the parent reports that their child is very specific or limited on how they will eat their food, this is a starting place for pushing their food limits and boundaries in the first couple of sessions.
Ask About Brands
Tip number 4 for completing a food eval is to consider different brands of foods that the child does and does not eat. This tip ties into Tip #3 when discussing the categories of foods. You want to know if the child will only eat a specific brand of food. This is common with cereal, snack foods, pizza, and pastas such as macaroni and cheese. It can happen with all foods, so it’s good to ask.
This may indicate that the child has challenges with processing novel experiences and may be easily distressed by change, from a sensory perspective. It also indicates that the child is very rigid in their thinking and expectations for mealtimes.
You will need to build confidence and trust, as something as small as changing brand of cereal might be a big leap.
during feeding evaluation: Ask About Temperature
Tip #5 for feeding evaluations is to think about the temperature of foods.
Another aspect to the sensory evaluation of food is the temperature of preferred foods. Ask how the child likes their food served–hot, cold or room temperature. While this may not seem like a big deal, but it can be for a child who is already struggling with introducing new foods and experiences into mealtimes.
It’s also a very personal preference, and by knowing that preference, you have an increased understanding of the child which leads to trust, and eventually a broadened food repertoire.
Sometimes the issue at hand is not the food at all. It is the learner’s difficulty getting it into the mouth. There are many choices when it comes to spoons, bowls, plates, cups, and serving ideas.
Check out some of these ideas to see if these may help your learner with self feeding or trying new food challenges.
Feeding therapy is complicated
Feeding therapy is complicated. Without the right knowledge and tools, therapist/parents can make the problems worse. Take time to get educated on correct feeding therapy techniques. In the meantime, feel free to engage your learner in messy play. This is a great first step to understanding and tolerating new foods.
Other areas to consider in a feeding assessment include:
- Anatomical considerations of the mouth and tongue
- Mobility of the jaw, tongue, lips, and cheeks
- Positioning and body posture
- Body awareness
- Developmental progression of oral motor skills
- Muscle considerations and issues that impact musculature (digit sucking, extended use of bottle or pacifier, reverse swallow/tongue trust, tongue, chewing habits, lip closure, vertical chewing during food prep stage,
- Structural abnormalities (teeth alignment, tongue tie, palate, tonsils, lip symmetry, etc.)
- Movements and range of motion in mouth, cheeks, lips, jaw: Jaw Thrust, Exaggerated Jaw Movements, Jaw Instability, Jaw Clenching, Tonic Bite, Jaw Retraction, Tongue Retraction, Tongue Protrusion, Stability Bite
- Alignment of teeth
- Presence of gagging or choking on foods
- Speech skills
- Sleep habits (sleeping through the night, snoring, light sleeper/heavy sleeper) Support sleep hygiene and even addressing newborns not sleeping through the night as sleep has a role in feeding routine and schedules.
- Tooth Grinding
- Phases of food swallow- Oral preparation, Oral Propulsion, Pharyngeal phase, Esophageal phase
- Vision and Visual motor skills
- Tone and musculature of the body-impacting range of motion, posture, etc.
- Fine motor skills
You’ll want to contact a pediatric occupational therapist who is experienced in feeding evaluations, including the oral motor aspect of food assessments.
Feeding Evaluations in the School Setting
While feeding evaluations are not typically done in the school setting for various reasons, there can be some components of feeding that a school based OT will address.
Specifically, the educational model of school based occupational therapy services simply means that feeding aspects may not impact the educational participation of the student. It will definitely depend on the specific needs of the individual, so there isn’t a one size fits all definition to feeding and schools.
For one thing, not all school based therapists are proficient in feeding therapy, and some aspects should be addressed in an outpatient setting under the medical model. And, feeding therapy and interventions can be pretty intensive, and are typically covered by insurance. While feeding is in the scope of occupational therapy’s practice, the risk for carryover, aspiration, and safety protocols for swallowing is simply too great. Feeding is an area of intervention where collaboration and carryover is essential, so the school cafeteria just might not be the safest place for this!
Some areas of feeding that might be addressed in the school setting include:
- OT can make accommodations for the child like where they sit or who is near them
- If gag reflux is present when sitting in the cafeteria, then maybe other accommodations are needed and OT can support this area.
- OT can provide calming strategies before, during, and after eating.
- OT absolutely can work with the student to make sure they can open food and lunch containers
- OT can provide seating opportunities for balance and posture when eating lunch
- OT can offer suggestions for getting on and off the cafeteria benches or lunch table seats, especially if motor planning is an issue.
- OT can support the self regulation and social aspects of feeding in the school cafeteria.
To address these areas and if you need information on how to request an OT eval in schools, start with our related blog posts.
Use the Food Inventory Tool- A Parent Report Screening Tool to incorporate into feeding evaluations to ensure successful feeding therapy.
This tool provides the therapist with a data sheet for a child’s repertoire allowing for consistent data collection over the course of feeding treatment. It also provides the therapist with a professional looking tool and talking point during the initial feeding evaluation to ensure that a comprehensive list of foods the child eats is gathered to support successful feeding therapy.
Click here to get a copy of the Food Inventory Tool- A Parent Report Screening Tool.

Contributor: Kaylee is a pediatric occupational therapist with a bachelors in Health Science from Syracuse University at Utica College, and a Masters in Occupational Therapy from Utica College. Kaylee has been working with children with special needs for 8 years, and practicing occupational therapy for 4 years, primarily in a private clinic, but has home health experience as well. Kaylee has a passion for working with the areas of feeding, visual development, and motor integration.
*The term, “learner” is used throughout this post for readability, however this information is relevant for students, patients, clients, children of all ages and stages or whomever could benefit from these resources. The term “they” is used instead of he/she to be inclusive.