In this post, we are going to give you the basics of Ayres Sensory Integration. If you have never heard of it, continue reading for plenty of information and resources that will help you become more familiar with this practice. Or, if you are trained in sensory approaches and looking to refresh your knowledge, we have got you covered. Learn more about the sensory system and and sensory-based activities in this resource on Sensory.
WHAT IS Ayres SENSORY INTEGRATION?
You may have heard the terms Ayres Sensory Integration, of Ayres SI. Maybe you’re familiar with the term sensory integration. But what do these terms mean?
Sensory integration has many layers, but it can be made quite simple. In fact, everyone has experienced sensory integration! Think about your senses; the way you feel things on your skin, see bright or dim light, smell a cup of coffee, or feel dizzy on a rollercoaster. Your body senses a stimulus, for example, the feeling of your shirt against your skin.
After a few moments, you don’t think about how the shirt feels on your skin. You wear it all day long without feeling it touch you.
This is an example of sensory integration. That sensation – the touch of the shirt to your skin – was processed and organized by your nervous system, and the nervous system decided that it did not need to process it any more. In other words, it was integrated!
But what happens if the sensation is not integrated?
You may have heard of someone who can feel their shirt, particularly the tag of their shirt, all day long. It may bother them so much that they cut off those tags to avoid feeling that sensation.
It may be that somewhere along the sensory nervous system pathway, the signals for processing that touch sensation are blocked, or lost. Instead of being processed and integrated as, “You don’t need to feel this any more!”, it’s stuck in a processing limbo of, “what is this that I am feeling?”.
Much like how a sudden closure on the freeway means that you will have to find another way to your destination, those sensory signals need to learn where to go when their path is not clear.
Sensory integration therapy can help find a new path to that destination and turn off the signals that cause the over-response to the stimuli (in this case, the shirt).
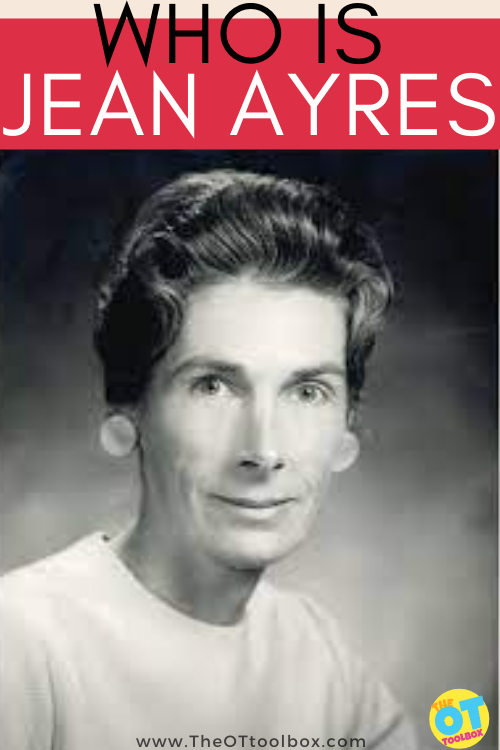
WHO IS Jean AYRES?
Dr. A. Jean Ayres, an occupational therapist, psychologist, and neuroscientist, developed this theory and practice in the mid 1970s. She recognized that a child’s sensory system can greatly impact how they perceive and interact with the world around them. Dr. Jean Ayres developed specific sensory integration interventions based on her research findings over the course of her career.
Since 2005, Ayres Sensory Integration (ASI) has been trademarked to differentiate this particular method from other sensory-based therapies. The term Ayres Sensory Integration, or ASI, encompasses the theory, assessments, and interventions that were developed by Dr. Ayres.
WHAT IS SPECIAL ABOUT Ayres Sensory Integration?
There are reasons why ASI is trademarked and other sensory approaches are not – so what makes Ayres Sensory Integration so unique? One reason why the trademark was necessary was to clarify to the public and the academic communities which evidence to correlate with ASI.
The evidence for sensory interventions were becoming increasingly mucky – it became difficult to discern if ASI worked because so many people were calling any sensory approaches ASI, even if they did not align with the principles (Parham et al., 2007).
To be considered true ASI, a trained practitioner must follow a specific protocol in their evaluation and treatment of their client. To start, the practitioner would evaluate their client using methods of naturalistic observation, conducting caregiver and teacher interviews, administering standardized testing, and performing clinical observations.
After the evaluation is complete, they will determine the ways in which sensory integration deficits may be interfering with the child’s functional performance.
Core Elements of Ayres Sensory Integration
After determining that ASI is an appropriate intervention method for a child, the trained practitioner will develop sensory interventions that fall within the core elements of the ASI approach:
- Ensures physical safety.
- Presents sensory opportunities.
- Helps maintain appropriate levels of alertness.
- Challenges postural, ocular, oral, or bilateral motor control.
- Challenges praxis and organization of behavior.
- Collaborates in activity choice.
- Tailors activity to present the just-right challenge.
- Ensures that activities are successful.
- Supports a child’s intrinsic motivation to play.
- Establishes a therapeutic alliance.
(Parham et al., 2020)
DOES Ayres Sensory Integration WORK?
Sensory integration is an on-going research topic in the field of occupational therapy. Many recent publications have suggested that ASI can be used to improve occupational performance (Koester et al., 2014; Miller, Coll, & Schoen, 2007; Pfeiffer, Koenig, Kinnealey, Sheppard, & Henderson, 2011; Roley et al., 2015; Schaaf & Nightlinger, 2007; Schaaf et al., 2013, Schaaf et al., 2015; Watling & Hauer, 2015).
In other words, ASI is supported by research in it’s main goal: to increase a child’s participation in their daily activities.
ASI was originally developed as a measure to address the functional abilities of children with learning and behavioral concerns. The positive outcomes of ASI have since been well-documented for children with Autism Spectrum Disorder, as well as for children with learning disabilities, ADHD, developmental delay, regulatory disorder, and developmental coordination disorder.
The theory and practice has also been modified for use with other populations and age groups, too!
Who Uses Ayres Sensory Integration?
Most recent research estimates that up to 95% of children with developmental delays or disabilities have deficits in sensory functioning (AOTA, 2017).
Additionally, it is estimated that sensory processing difficulties occur in 5% to 14% kindergartners, 16% of elementary students, and 10% to 12% of people of all ages with no related diagnosis (AOTA, 2017).
In short, the relevance for sensory integration is huge, due the prevalence of sensory deficits in individuals of various populations.
To find out if an individual can benefit from ASI therapy, the Sensory Integration and Praxis Test (SIPT) would be administered, per the ASI guidelines. The SIPT was developed by Dr. Ayres specifically to test whether or not ASI is appropriate for an individual, and to highlight specific deficits in sensory processing.
RESOURCES on Sensory Integration
There are many great resources available for practitioners and families alike. See the options below to discover more about the sensory system, ASI theory, and sensory-based interventions.
- Frequently Asked Questions about ASI
- How to Build Competency in ASI for Practitioners
- Sensory Integration Global Network
Want to become certified in ASI? The Collaborative for Leadership in Ayres Sensory Integration (CLASI) or ASI Wise are great places to start. - If you are looking for even more ASI information, look no further than this video! Occupational therapist Ivan describes the sensory system and methods of intervention in a way that I believe any one can understand.
- For a more advanced understanding of the neurological basis of ASI, check out this video.
Ayers Sensory Integration and Therapy
While Sensory integration (SI) refers to a theory developed by Dr. Jean Ayers in the 1960’s much has changed in the world since the conception of sensory integration therapy.
We have screens, online worlds, technology, fast paced lifestyles, full schedules, various educational models and programming types, changed environments, different home lifestyles, adapted parenting styles, and many other overall lifestyle differences since the 1960s.
The theory that our Central Nervous System (CNS) takes information from the outside world that has VASTLY changed, while our internal systems has not is an interesting one to chew on.
We’ve had to accommodate for these different and updated needs that our world has moved into.
What hasn’t changed is the nervous system’s ability t take information from the outside world, organize it, and use that information to produce purposeful and useful responses toward specific goals we have, physically, cognitively, emotionally, and behaviorally.
We are able to use that purposeful information in order to perceive incoming sensory information (the sensory systems of touch, movement, pressure, sounds, tastes, joint sense, sights, and internal information) in order to determine the quality of the responses of each sensory system as they work together as a whole.
It’s amazing when you think about it, right?!
Then, there is the vast amount of knowledge that we have as individuals. Today, we can access information, the use of AI, and we can share that information in seconds. Today, the awareness of tools and underlying reasons why we behave the way we do is available to every individual.
This might mean that sensory interventions can be used in not just the clinical setting anymore. Jean Ayres layed the framework for this knowledge and theories.
References on Jean Ayers Sensory Integration
The following are sources of information regarding Jean Ayers Sensory Integration.
For more in-depth information on Jean Ayres’ sensory integration theory and a comprehensive exploration of occupational therapy interventions based on her principles, I recommend referring to authoritative textbooks, academic papers, and professional resources in the field of sensory integration therapy. These references can provide valuable insights and guidance for those seeking a deeper understanding and effective application of Ayres’ groundbreaking concepts in occupational therapy practice.
American Occupational Therapy Association [AOTA]. (2017). Frequently asked questions (FAQ) about: Ayres Sensory Integration®. https://www.aota.org/-
/media/Corporate/Files/Secure/Practice/Children/FAQAyres.pdf
Koester, A. C., Mailloux, Z., Coleman, G. G., Mori, A. B., Paul, S. M., Blanche, E., … Cermak, S. A. (2014). Sensory integration functions of children with cochlear implants. American Journal of Occupational Therapy, 68, 562–569.
http://dx.doi.org/10.5014/ajot.2014.012187
Miller, L. J., Coll, J. R., & Schoen, S. A. (2007). A randomized controlled pilot study of the effectiveness of occupational therapy for children with sensory modulation disorder. American Journal of Occupational Therapy, 61, 228–238.
Parham, L. D.., Smith Roley, S., May-Benson, T. A., Koomar J., Brett-Green, B., Burke, J. P., Cohn, E. S., Mailloux, Z., Miller, L. C. & Schaaf, R. C. (2020). Development of a fidelity measure for research on the effectiveness of the Ayres Sensory Integration® intervention. American Journal of Occupational Therapy, 65, 133-142. https://doi.org/10.5014/ajot.2011.000745
Parham, L. D., Cohn, E. S., Spitzer, S., Koomar, J. A., Miller, L. J., Burke, J. P. … Summers, C. A. (2007). Fidelity in sensory integration intervention research. American Journal of Occupational Therapy, 61, 216–227.
Pfeiffer, B. A., Koenig, K., Kinnealey, M., Sheppard, M., & Henderson, L. (2011). Effectiveness of sensory integration interventions in children with autism spectrum disorders: A pilot study. American Journal of Occupational Therapy, 65, 76–85. http://dx.doi.org/10.5014/ajot.2011.09205
Roley, S. S., Mailloux, Z., Parham, L. D., Schaaf, R. C., Lane, C. J., & Cermak, S. (2015). Sensory integration and praxis patterns in children with autism. American Journal of Occupational Therapy, 69, 6901220010. http://dx.doi.org/ 10.5014/ajot.2015.012476
Schaaf, R. C., Benevides, T., Mailloux, Z., Faller, P., Hunt, J., van Hooydonk, E.,… Kelly, D. (2013). An intervention for sensory difficulties in children with autism: A randomized trial. Journal of Autism and Developmental Disorders, 44, 1493–1506.
http://dx.doi.org/10.1007/ s10803-013-1983-8
Schaaf, R. C., Cohn, E. S., Burke, J., Dumont, R., Miller, A., & Mailloux, Z. (2015). Linking sensory factors to participation: Establishing intervention goals with parents for children with autism spectrum disorder. American Journal of Occupational Therapy, 69, http:// dx.doi.org/10.5014/ajot.2015.018036
Watling, R., & Hauer, S. (2015). Effectiveness of Ayres Sensory Integration® and sensory-based interventions for people with autism spectrum disorder: A systematic review. American Journal of Occupational Therapy, 69, 6905180030.
http://dx.doi.org/10.5014/ajot.2015.018051

Sydney Thorson, OTR/L, is a new occupational therapist working in school-based therapy. Her
background is in Human Development and Family Studies, and she is passionate about
providing individualized and meaningful treatment for each child and their family. Sydney is also
a children’s author and illustrator and is always working on new and exciting projects.