In this blog post, we are addressing trauma informed occupational therapy, including trauma informed interventions and how to take a trauma informed approach in occupational therapy.
Imagine your mental, physical, and emotional health as a backpack. Some days, that backpack may be really heavy, full, and wear you down. Other days, it may be a bit lighter, and you are quicker on your feet, but the backpack is always there. This is the visualization of health that I think is just perfect when discussing trauma-informed occupational therapy practice.
Trauma Informed Care: the hypothical backpack
Everyone wears this hypothetical “backpack”; young and old, rich and poor. It’s up to us as health care professionals, to do our best to consider what we know about what load a person is carrying, while knowing that we won’t ever fully understand someone’s story.
Included in this “loaded backpack” is the connection between emotional regulation and executive functioning skills, where both emotions and the ability to self regulate, impacts cognitive actions.
Having an awareness of this emotional health, allows one to shift perspectives on how one behaves, acts, speaks, and functions. Cognitive and emotional health can be a large factor of someone’s overall health.
WHAT IS TRAUMA-INFORMED PRACTICE?
It’s important to understand the definition of trauma informed practice.
The effects trauma and adverse childhood experiences have on a person have been understood for some time now. Infant, child, and adolescent mental health is still a growing field.
The “backpack” visual helps to remember that even though occupational therapists may not work in a mental health setting, an individual still carries their traumatic history, anxiety, or depression as they walk into your office.
Trauma informed care is different than trauma-specific interventions. Where trauma informed refers to the awareness and recognition of various traumas and the impact of organizations or systems impact individuals, families, groups, communities, etc. the specific interventions address assessments, treatments, and specific recovery supports to impact trauma.
Example of Trauma Informed occupational therapy
Take 5-year-old ‘Thomas’ as an example. His aunt brings him to therapy at your outpatient clinic, and you notice that he is really shy and resistant to join you in a treatment room.
Thomas was referred to OT for delayed fine motor skills, but you are unable to convince him to do much with his hands at all. He won’t even look at you for more than one second.
After a few sessions pass, and there are no improvements in his participation, you ask the aunt how things are going at home, and learn a new perspective about Thomas’ overall health. You still must provide services for his fine motor skills, but now you do so through a new lens that respects, and includes his needs as a child with a traumatic history.
An individual’s traumatic history may not be the reason they are seeking services, but it should always be considered, and assess for. Traumatic experiences shape the way we perform our occupations.
The trauma response and/or triggers should be considered in all aspects of practice; when writing treatment plans, speaking to the individual and their family, and designing the treatment environment.
This is trauma-informed occupational therapy practice in a nutshell.
GUIDELINES FOR TRAUMA-INFORMED Occupational Therapy
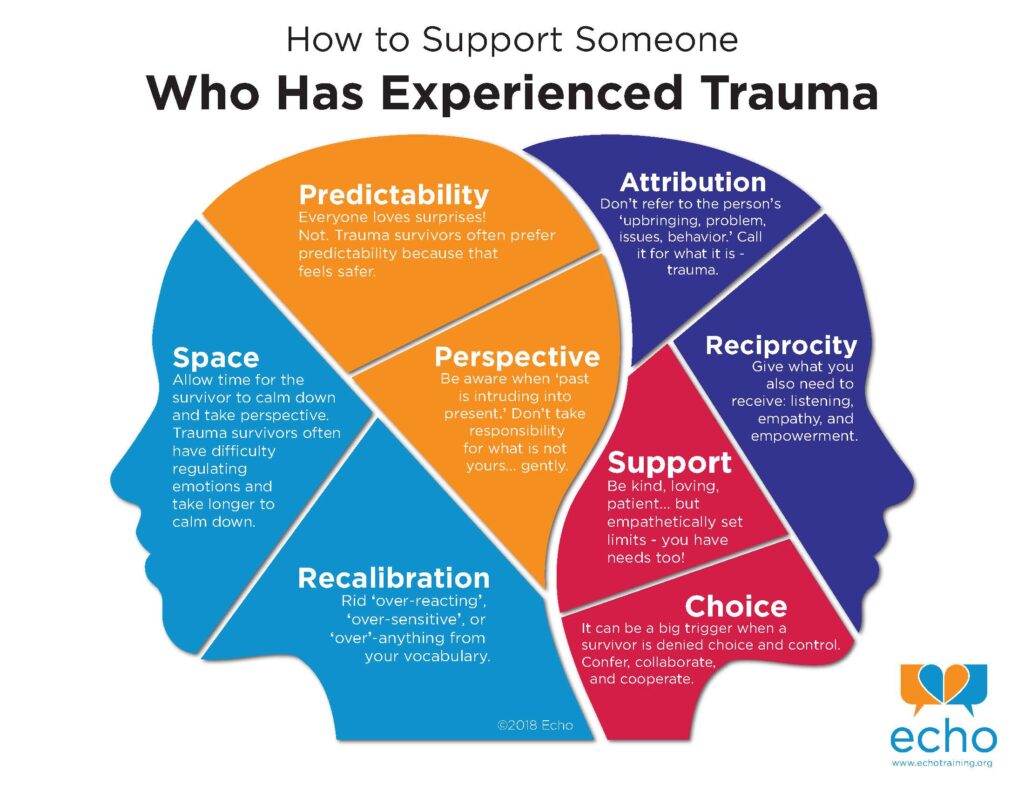
How will you adjust your services to meet the unique needs of an individual who has experienced trauma?
“Given the long-term effects of adverse experiences in childhood, it is particularly important that all disciplines working in health care assess trauma; address safety in schools and the community; build strengths and resilience; and provide opportunities for educational, economic, and social successes” (AOTA, 2019).
Evidenced-based practice is always the best place to start. The AOTA’s guidelines from the May 2019 continuing education article Understanding and Applying Trauma Informed Approaches across Occupational Therapy Settings, breaks down trauma-informed practice in occupational therapy. This resource highlights best-practice standards from the Substance Abuse and Mental Health Services Administration (SAMSHA).
6 Trauma-informed Principles:
The 6 principles of trauma informed care are as follows:
1. Safety
2. Trustworthiness and transparency
3. Peer support and mutual self-help
4. Collaboration and mutuality
5. Empowerment, voice, and choice
6. Cultural, historical, and gender issues.
The table below is a modifed version of Figure 1 from the AOTA (2019) article. It provides examples of what to do and what not to do in accordance with the principles above.
Trauma Informed Occupational Therapy Do’s and Don’ts
Table Adapted From Figure 1, AOTA (2019)
| Do | Don’t | Principle |
| Ask permission before doing anything. | Assume an individual’s comfort level. | #1 Safety #4 Collaboration and mutuality #5 Empowerment, voice, and choice |
| Acknowledge what you cannot change | Ignore things over which you cannot control | #2 Trustworthiness and transparency |
| Always ask preferred pronouns | Assume based on appearance, etc. | #6 Cultural, historical, and gender issues |
| Recognize that trauma manifests in many different ways. | Automatically attribute challenging behaviors to personality | #1 Safety |
Becoming a trauma-informed provider is not an easy shift for everyone. Considering the current pressures that healthcare professional face, having to adapt towards trauma-informed care is not always supported by staff or administration.
The AOTA provides resources and valuable information for occupational therapists based on the setting they work in.
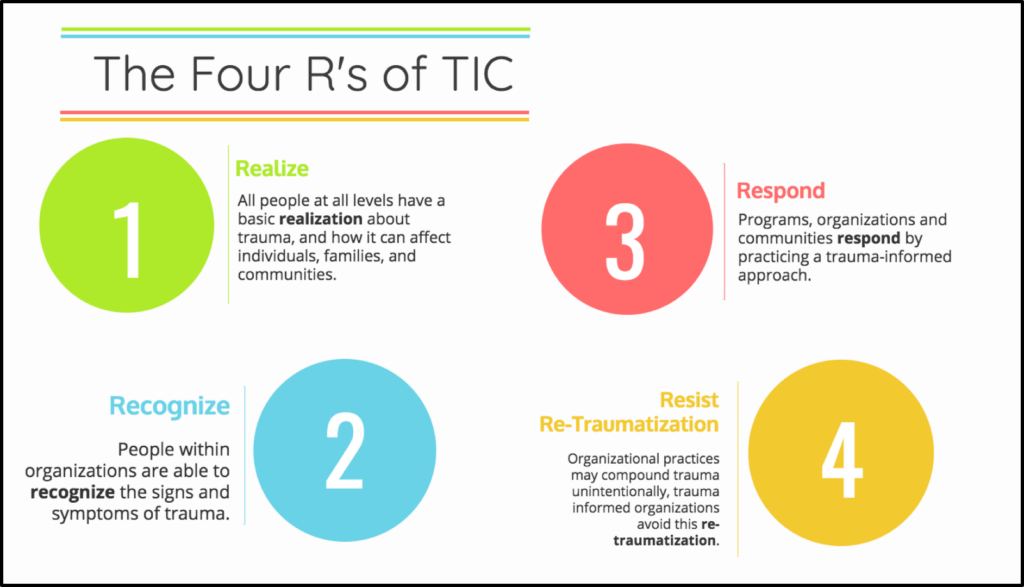
The table above takes into consideration, the Four R’s of Trauma Informed Care: realize, recognize, respond, and resist re-traumatization.
Trauma Informed Strategies for Occupational Therapy
Many of the following guidelines will assist all healthcare providers, educators, and caregivers in learning trauma-informed practices.
Early Childhood Settings: Increase Collaboration to Promote Prevention
- Promote early bonding through skin-to-skin, kangaroo care, private rooms, and opportunities for parent decision-making
- Increase the amount of collaboration with all involved, and identify the barriers to involving family members in the care of their child
- Celebrate family advocates
- More ideas and resources are available at Zero to Three, The Center of Excellence for Infant and Early Childhood Mental Health Consultation, and Think Babies
School Settings: Recognizing Common Trrauma-based Responses
- Trauma has negative effects on learning, and should be addressed school-wide (not just for students who receive special education)
- AOTA suggests that OTs frame school behaviors through a lens that recognizes potential triggers and responses
- Common traumatic stress behaviors include: “intrusive thoughts, irritability, arousal, anxiety, fear, difficulty concentrating, sensory dysregulation, aggression against self and others, dissociative symptoms, somatization, and character issues” (AOTA, 2019)
- Trauma-Sensitive Schools Training Package
- Online training offered by the National Center for Safe, Supportive Learning Environments.
- AOTA reports using this training as a Tier 1 intervention, educating the staff and ensuring common understanding.
- Cognitive Behavioral Intervention for Trauma in Schools (CBITS) intervention
- Created by Wong and colleagues specifically to target children subjected to community violence
- Suggested use as a Tier 2 or targeted intervention
- Trauma-Focused Cognitive Behavioral Intervention (TF-CBT)
- Similar to the above, but suggested practice in Tier 3 intervention, including students and their families, in collaboration with community mental health providers.
The AOTA (2019) offers more information about occupational therapy’s role in trauma-informed care in various settings, including primary care, community, residential, and foster care settings.
Regardless of the setting, location, or age group you may work with, trauma-informed practice is necessary.
We hope this article gave you some insight on a very important topic, and ideas on how to incorporate trauma informed care it in your practice – wherever you are. What will you do to move towards a trauma-informed practice?

Sydney Thorson, OTR/L, is a new occupational therapist working in school-based therapy. Her
background is in Human Development and Family Studies, and she is passionate about
providing individualized and meaningful treatment for each child and their family. Sydney is also
a children’s author and illustrator and is always working on new and exciting projects.


