An open thumb web space ensures a functional grasp on the pencil and is an important fine motor skill. When the thumb is squashed against the pencil and the index finger, it is difficult to control the pencil with small motor movement changes. These activities are designed to promote an open thumb web space. Why not try using them before a handwriting task to warm up the hands?
This paper clip activity prompts opposition of the thumb with an open thumb web space. Games with paper clips are a great way to target an open thumb web space.

What is Hand Web Space?
Let’s start by covering thenar web space and the definition of hand web space. The thumb web space is that space between your thumb and pointer finger that makes an “O” when you make the “OK” sign. It’s the first web space, which opens in a spread open palm. This area is also known as the thenar space.
The web space is that area between the thumb and the index finger.
In order to grasp small items with your thumb and index finger, you need to oppose the tip of your thumb to the tip of your pointer finger. Not only do the tips of the fingers need to touch, but the thumb must rotate at the joint closest to your hand. This opposition is needed to manipulate and grasp small items like shoe laces, buttons, and zippers.
In the hand, there are several anatomical features that impact web space:
- Thenar eminence– (The bulk of the muscles at the base of the thumb, in the palmar area)
- Thenar muscles- the abductor pollicis brevis, the flexor pollicis brevis, and the opponens pollicis
- Carpal bones
- Metacarpal bones
- Phalangeal bones
- Lumbricals- The main role of the lumbrical muscles is to straighten the fingers to straighten and help bend the MCP joints.
- Intrinsic Muscles- Also known as the thenar muscles. In the role of the thumbweb space, the intrinsic muscles include: adductor pollicis, flexor pollicis brevis, abductor pollicis brevis, opponens pollicis. These are muscles that originate and end within the hand.
- Median nerve– the nerve that innervates the thenar muscles, with the exception of the deep head of flexor pollicis brevis and adductor pollicis muscle, which receive their innervation via the ulnar nerve.
- Long Flexor Tendons- Tendons that originate outside of the hand, in the forearm of the upper extremity. These muscles bend the wrist forward toward the palm.
- Extrinsic Muscles- Muscles that originate in the forearm of the upper extremity. Extrinsic muscles include the flexors and the extensors.
- Long Flexor Muscles- Flexor Pollicis Longus and Abductor Pollicis Longus.
- Long Extensor Muscles- The extrinsic extensors make up the border of the anatomical snuff box: Extensor pollicis longus, Extensor pollicis brevis, and Abductor pollicis longus
Closed Web Space in the Hand
Closed web space occurs when the thumb is squashed up against the side of the index finger during functional tasks.
When kids write or color with that web space area squashed shut, it’s a sign of problems. There may be limited dexterity and precision in fine motor tasks when a closed web space is present.
Then, as a result, there might be compensating for thumb instability, underdeveloped hand arches, and/or poor strength. Each of these problem areas will lead to difficulties with handwriting, dexterity, manipulation of small items like beads, and pencil grasp.
Writing with a closed web space is inefficient and will cause poor and slow handwriting, especially as kids grow and are expected to write at faster speeds. A closed web space while attempting to manage fasteners such as buttons and zippers will lead to fumbling and difficulty.
Web hand space includes two components:
- Opposition with rotation of the thumb at the CMC joint
- Flexion of the distal joints of the thumb (MCP joint and IP joint)
Opposition with Rotation- Related to hand web space is opposition of the tip of the thumb to the tip of the pointer finger. This blog post covers more on opposition with a fine motor paper clip activity.
When opposing objects with the thumb and pointer finger, the thumb’s thenar muscles work to oppose with a nice, rounded web opening during functional tasks. This is needed for advancing and positioning a pencil when writing, precision tasks such as threading a needle. stringing beads, closing a plastic sandwich bag, managing a button with ease, and pulling a zipper.
With a closed thumb web space and lateral pinch of the thumb versus true opposition, a child will fumble.
Flexion of Thumb Joints- Also related to thenar web space, or open thumb web space is the flexion of the joints of the thumb. Flexion, or a bent position, allows the thumb to bend toward the palm at the joints in the thumb.
- The CMC joint-CMC joint refers to carpo-metacarpal joint. Also known as the basal joint, or the saddle joint. This joint is located between the trapezius of the carpal joints in the wrist and the metacarpal in the first digit. There are three movements completed by the CMC joint:
- Flexion- When the CMC joint moves in isolation, the thumb is able to flex, or bend, across the palmar area to touch the base of the pinkie finger, or the small finger of the hand.
- Rotation- This joint also enables rotation to oppose the fingertips.
- Abduction/Adduction- Abduction spreads the thumb away from the second finger and creates a wide web space. Adduction brings the thumb back to the second finger to close the thumbweb space.
- The MCP Joint- The MCM joint is the metacarpophalangeal joint. This joint is located between the metacarpal bone and the proximal phalangeal bone in the thumb. When the MCP joint bends in isolation, the joint at the base of the web space across the palm to touch the base of the pinkie finger (5th digit, or small finger).
- The IP Joint- The IP joint is the interphalangeal joint. This joint is located between the proximal pharynx and the distal pharynx of the thumb. When the IP joint works in isolation, only the tip of the thumb bends.
This blog post on a thumb wrap exercise covers more on thumb flexion and the flexion of the individual joints that impact functional grasp on a pencil during handwriting.
web space hand functions
An open thumb webspace is necessary for tasks requiring in-hand manipulation such as moving coins from the palm to the fingertips. If the thumb is squashed up against the index finger, it can not be helpful in manipulating items.
An essential part of a functional open thumb webspace is a flexed thumb IP joint. Read more about this simple tip for a functional pencil grasp that encourages a flexed IP joint.
RELATED READ: Here are activities and tools to address pencil grasp.
Fine Motor Activities to Improve Open Thumb Web Space
These web space hand activities will help improve an open web space for functional grasp:
1. Using a flexed IP joint of the thumb while encouraging thumb opposition is the number one best way to encourage an open thumb web space. The resulting rotation of the thumb and a tip-to-tip grasp will result in an open space that allows for improved dexterity.
2. Beading Activities- This activity with small beads and play dough is an easy way to strengthen these skills.
3. Fine Motor Crafts- Make and Take made these caterpillar pets that address bilateral coordination and an open thumb web space when threading the pony beads.
4. Threading Activities- Thread beads onto feathers like we did in this fine motor beading activity.
5. Tweezer Activities- Use homemade craft stick tweezers to encourage an open thumb space. Tweezer Games like Operation are a great way to work on this skill. Tweezer activities promote an open web space and stabilization of the thumb.
6. Lacing Activities- Encourage an open thumb web space during lacing activities, like in this DIY lacing activities.
Here are more lacing card ideas that you can use to promote an open web space.
7. Pegboard Activities- Use a homemade pegboard to encourage an open thumb web space.
Web Space Hand Activities
An important piece of an open thumb space is the components that make up the skill. These include arch development, opposition of the thumb to the pointer finger, rotation of the thumb CMC joint, and flexion of the MCP and IP joints.
To encourage arch development try these web space hand movements try these activities:
- Tearing small pieces of paper
- Shaking dice within the hand
- Rolling small pieces of play dough into balls
To encourage opposition of the thumb to the pointer finger and rotation of the thumb CMC joint, a child needs strength in the muscles of the thumb. The bulk of the thenar eminence allows for rotation, control, and endurance in activities with sustained thumb rotation.
Remember, while completing these activities, encourage the child to flex the thumb IP joint and to rotate the thumb to oppose the fingers. This promotes an open thumb web space, and not a squashed space!
- Pushing small pegs into a pegboard
- Pinching clothes pins
- Tweezer activities
- Popping bubble wrap
- Connect 4 game
- Using an eye dropper to transfer water
- Stringing beads
- Wind-up toys
A few toys that help encourage an open web space:
Amazon affiliate links are included below:
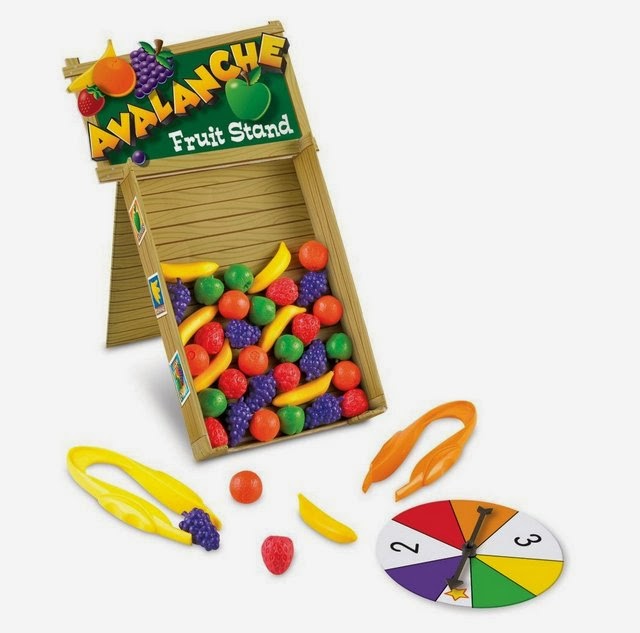
This Avalanche Fruit Stand from Learning Resources is a colorful way to encourage an open web space. The vertical surface is perfect for encouraging an extended wrist (see below).
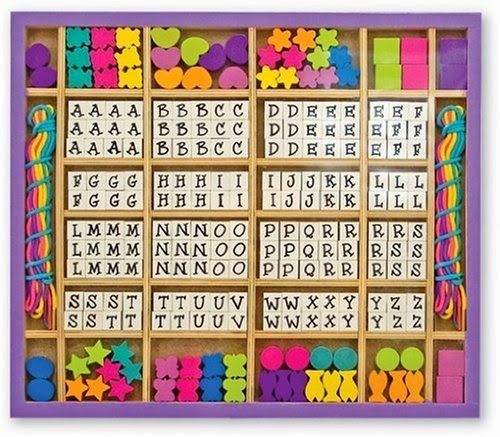
Bead Sets: Stringing beads is a good way to encourage an open web space. The child must hold the bead and string between their thumb and index fingers. Collapsing of the thumb web space will happen when the child demonstrates weakness in the muscles of the thumb. Beading is a repetitive activity and promotes strength.
This Melissa & Doug Deluxe Wooden Stringing Beads with over 200 beads from Melissa & Doug has over 200 beads in different colors and shapes, and even letters! You could even form sentences for the child to copy and practice their improved pencil grasp!
Rock ‘Em Sock ‘Em Robots: Often times, a child will wrap their thumb around the index finger when they are writing with a pencil. This indicates instability in the thumb and the muscles that allow for smooth pencil motions. Pushing down on the buttons of the Rock ‘Em Sock ‘Em ROBOTS Game from Mattel really strengthens the muscles of the thumb and allows for more stability leading to an open web space and ultimately more fluid motions of the pencil in letter formation. Plus, this game is just plain old FUN for kids of all ages!

More thumb web space hand activities
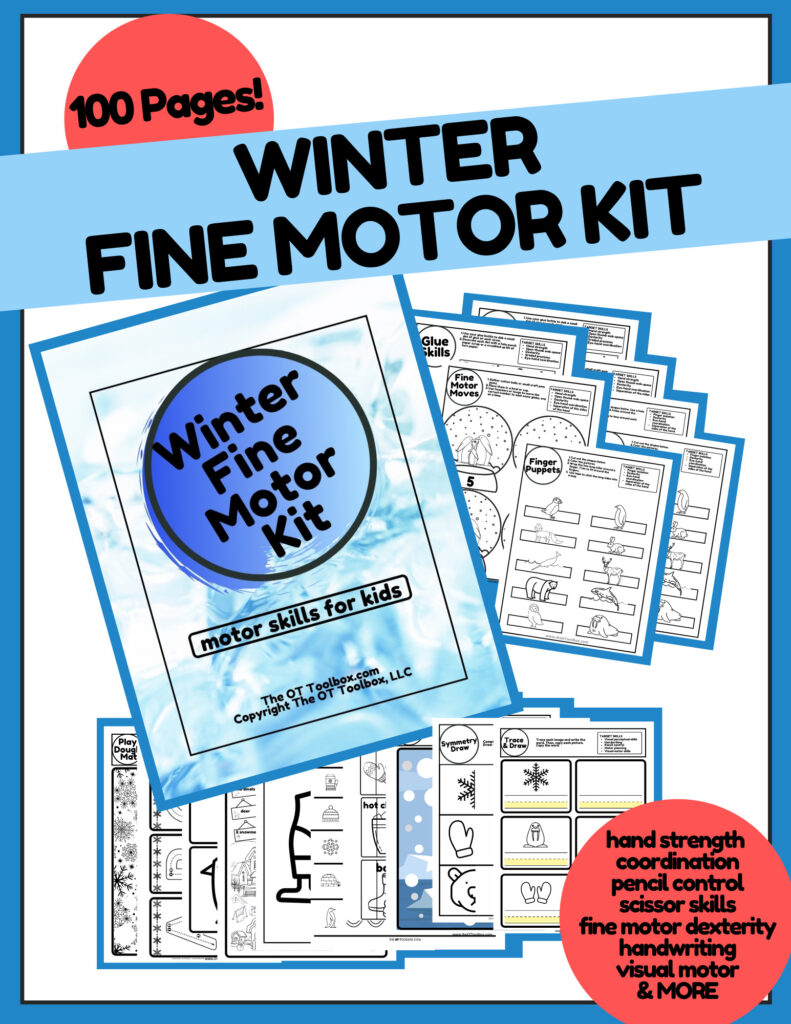
We’ve created many fine motor kits with lacing, pinch and crumbling paper activities, and tools to support fine motor development of the thumb web space:
Working on fine motor skills, visual perception, visual motor skills, sensory tolerance, handwriting, or scissor skills? Our Fine Motor Kits cover all of these areas and more.
Check out the seasonal Fine Motor Kits that kids love:
Or, grab one of our themed Fine Motor Kits to target skills with fun themes:
- Frogs Fine Motor Kit
- Unicorns Fine Motor Kit
- Vehicles Fine Motor Kit
- Apple Fine Motor Kit
- Back to School Kit
- Sports Fine Motor Kit
- Outer Space Fine Motor Kit
- Fairytale Fine Motor Kit
- Plus more in our shop!
Want access to all of these kits…and more being added each month? Join The OT Toolbox Member’s Club!

Colleen Beck, OTR/L has been an occupational therapist since 2000, working in school-based, hand therapy, outpatient peds, EI, and SNF. Colleen created The OT Toolbox to inspire therapists, teachers, and parents with easy and fun tools to help children thrive. Read her story about going from an OT making $3/hour (after paying for kids’ childcare) to a full-time OT resource creator for millions of readers. Want to collaborate? Send an email to contact@theottoolbox.com.