For the child with sensory challenges, the classroom can be an overwhelming place. All of the sensory systems are touched on in the classroom. When sensory systems are challenged, learning is a struggle. School based OTs are often times consulted when students struggle with physical or sensory issues that result in educational deficits.
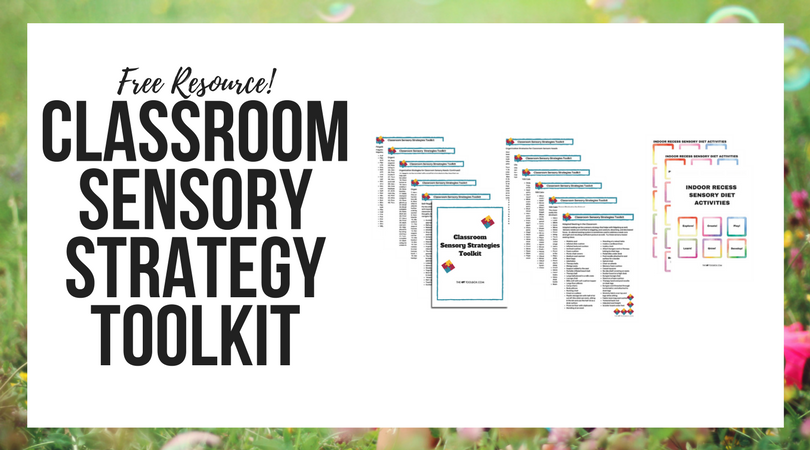
Previously, The OT Toolbox has shared free ways to incorporate sensory motor experiences into the classroom. You might be looking for more resources that can be used to address many sensory needs in the classroom. Below are sensory resources for the school based occupational therapist and strategies that can be incorporated into OT in the school.
These are strategies to fill your therapy toolbox and address everything from inattention to sensory meltdowns.
Sensory Resources for the School Based OT
This is a great article written on sensory integration practices in the school setting. It includes the clinical reasoning and practices that go along with sensory practice in the school. Of interest are sensory screening and evaluation recommendations for school settings, sensory intervention and treatment delivery options, and recommendations. Also included is a table with approaches and sensory strategies for Occupational Therapy intervention in the classroom or school setting.
Case studies include IEP goals or 504 accommodations related to sensory processing interventions.
Assessments for sensory needs can include direct observation of the child’s performance in the school setting. Observing a variety of tasks during the school day can be helpful to analyze the demands of specific activities, including needs and strengths in tool use, fatigue, sequencing, spatial concepts, social interactions, physical requirements, cognitive abilities, etc. A child transitions through a variety of settings during a school day and is challenged in various environments which might present differing needs or abilities. The school-based OT should assess a student’s sensory and neuromuscular functioning in these various environments.
Many students who struggle with sensory challenges benefit from a sensory diet during the school day. This specialized diet of sensory activities and input should be designed by an occupational therapist who assesses and identifies the student’s particular needs and strengths or interests. Sensory diets in the school can include many different tools, not limited to fidget tools, specialized seating, movement breaks, weighted lap pads or vests, calming scents, limited or structured visual adjustments, chewing tools, or other activities. Read more about the goals of a sensory diet.
Use this free Sensory Processing Disorder booklet for passing on sensory processing information to parents and teachers.
Fidgeting Tools for the Classroom
Fidgeting with items can help with attention, regulation, and focus. Try these fidgeting options in the classroom:
- DIY Fidget Tools
- Desk Fidget Tool for School
- DIY Pencil Topper Fidget Tool
- DIY Weighted Fidget Tool
- Help for Fidgeting During Homework
Adapted Seating in the Classroom
Adapted seating can be a sensory strategy that helps with fidgeting as well. Sensory needs can overflow to wiggling, poor posture, slouching, and decreased focus. An altered seating system is sometimes used to address a weak core strength and resulting inefficient posture as well. Try these sensory-based seating ideas:
- Cheap Alternative Seating Option
- Movement seats like a disk cushion are great for allowing movement for improved attention.
- Wobble Seat uses the idea of a therapy or stability ball in the form of a stool. This is great for classroom use because the giant therapy balls tend to roll away from desks.
- This Guide to Alternate Seating is a resource that can benefit many individuals in the school, including teachers, administrators, paraprofessionals, and school-based therapists.
- Special cushions
- Bean bags
- Intertubes
- Therapy balls
- Wedge seats
- Support added to the seat
- Etc.
Self-Regulation in the Classroom
- This guide is a Review of the Literature related to Self-Regulation in the Classroom.
- This site includes many different games and activities for self-regulation, including those designed to promote improved refocusing, relaxation, emotional regulation, impulsivity reduction, response regulation, and transitions in the classroom.
- Impulse control is a big struggle in the classroom or school environment. Here are strategies that can help with impulse control, a free printable sheet of impulse control strategies, and a printable impulse control journal.
- A quiet space or corner of the classroom can be a strategy that addresses many sensory needs.
- The Alert Program is a guide to teach and promote self-regulation.
- Zones of Regulation is a curriculum designed to help students recognize and address self-regulation needs.
Sensory-Based Interventions for the School Based OT
Sensory Integration Approach to School Based OT
Chewing Tools for Classroom Sensory Needs
- Pencil Topper Chews come in a variety of textures and toughness to meet sensory needs.
- Chewable jewelry is often times appropriate for the classroom, because the variety of necklace or bracelet styles on the market are discreet while meeting sensory needs.
- Here is information on how to choose the right chew tool for addressing sensory needs.
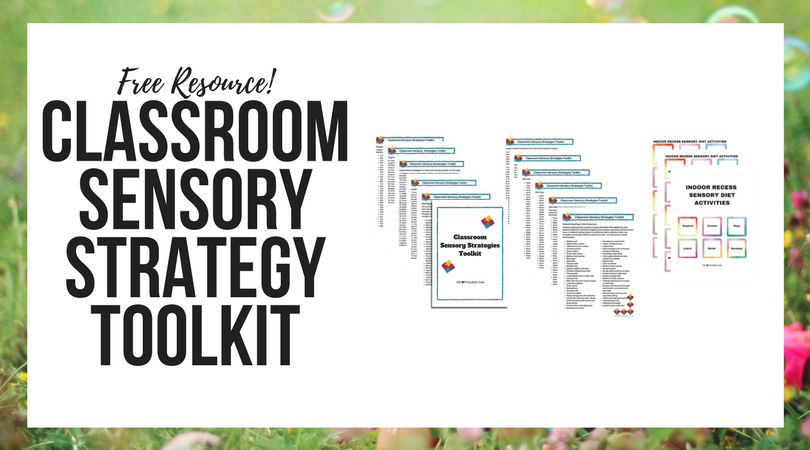
Push In or Pull Out OT Services in the School
-
Fidgeting Tools for the Classroom
-
Adapted Seating Strategies for the Classroom
-
Self-Regulation in the Classroom
-
105 Calm-down Strategies for the Classroom
-
Chewing Tools for Classroom Needs
-
45 Organizing Tools for Classroom Needs
-
Indoor Recess Sensory Diet Cards

Colleen Beck, OTR/L has been an occupational therapist since 2000, working in school-based, hand therapy, outpatient peds, EI, and SNF. Colleen created The OT Toolbox to inspire therapists, teachers, and parents with easy and fun tools to help children thrive. Read her story about going from an OT making $3/hour (after paying for kids’ childcare) to a full-time OT resource creator for millions of readers. Want to collaborate? Send an email to contact@theottoolbox.com.