Have you ever considered what a wealth of sensory input there is in outdoor sensory play? Here, you’ll find outdoor sensory activities that would make a great addition to outdoor occupational therapy sessions, or just sensory input through playing outdoors! Consider taking the benefits of sensory play and moving them to an environment with differences in sounds, temperatures, textures, surfaces. You end up with a functional space that invites motor and sensory development!
Previously, we’ve shared how to go on a sensory nature walk, but this resource covers much more in the way of outdoor occupational therapy activities to support needs.
Outdoor Sensory Activities
The outdoor sensory ideas listed below include sensory activities that can naturally be found outdoors!
It’s a fact that kids are spending less time playing outdoors. From after-school schedules to two working parents, to unsafe conditions, to increased digital screen time, to less outdoor recess time…kids just get less natural play in the outdoors.
Research on outdoor sensory play tells us that playing outdoors supports development through areas such as: developmental and primary tasks that children must achieve can be effectively improved through outdoor play. These include: exploring, risk-taking, fine and gross motor development, absorption of basic knowledge, social skills, self-confidence, attention, language skills, among others.
In fact, one study found a sensory diet in outdoor play along with sensory integration therapy resulted in better functional behavior of kids with ADHD (Sahoo & Senapati).
Some therapists have connected the dots between less outdoor play and increased sensory struggles and attention difficulties in learning. Knowing this, it can be powerful to have a list of outdoor sensory activities that can be recommended as therapy home programing and family activities that meet underlying needs.
A note about using outdoor activities in sensory diets (and creating a sensory lifestyle…)
Sensory activities can be prescribed according to need along with environment in order to maximize sensory input within a child’s day such at home, within the community, during transitions, or within the school day. Outdoors are part of our everyday. Whether it’s walking to the car or school bus, travelling down a sidewalk, or spending time outside in the yard, there are many opportunities to support sensory and emotional regulation needs with outdoor play.
Using authentic sensory input within the child’s environment plays into the whole child that we must understand when focusing on any goal toward improved functional independence.
We’ve been talking a lot about sensory diets here on The OT Toolbox recently. Understanding what a sensory diet is and how it can be used within a sensory lifestyle is a big part of integrating sensory activities and sensory play into needed sensory input that a child needs to self-regulation, cope with his or her environment, and to attend or focus despite sensory overload or distractions.
You’ll find more outdoor sensory diet activities like these outdoor sensory diet activities for the backyard coming to the site very soon!
For specifics on how to get started with a sensory diet, and how to use these outdoor sensory processing strategies in a sensory plan, start here with this resource on how to create a sensory diet.
Outdoor sensory activities can be specific to sensory system like proprioception activities, auditory processing, vestibular sensory diet activities, and the rest of the sensory systems.

Outdoor occupational therapy
When therapists develop a specific and highly individualized sensory diet, it’s not just throwing together a day filled with sensory input. It’s activities based on sensory need and strategizing. Each of the nature-based sensory activities above should meet specific needs of the child.
Imagine a world with more creative outdoor play that involves a variety of enriching sensory input. The proprioceptive input from running and jumping into puddles can calm the child who is typically overactive.
Outdoor occupational therapy supports the development of skills in a functional and natural space. When OTs venture outdoors for therapy practice, the world opens up in the way of sensory input, motor experiences, emotional regulation, and skill-building.
Occupational therapists practice outdoors for many reasons:
- Develop confidence
- Social skill building
- Independence with clothing
- Attention
- Focus
- Body awareness
- Problem solving
- Executive functioning skills
- Safety skills
- Motor planning
- Sensory processing
- Connection with others
Through outdoor occupational therapy, individuals experience all that nature has to offer while developing skills, just like one would in traditional occupational therapy services.
Below, you’ll find specifically sensory occupational therapy activities that can occur outdoors.
Sensory Activities for Outdoors
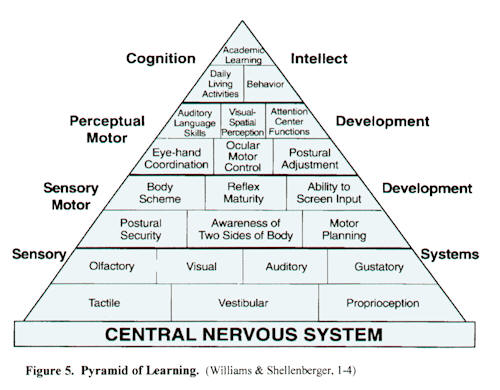
Nature, playing outdoors, and experiencing everything the outdoors has to offer supports all of the sensory systems. Let’s break this concept down:
- Visual System- Outside, we can see details in the trees, notice differences in plants, spot items hidden in the grass. Vision is more than just acuity. It’s through the visual sense that we learn, communicate. Visual motor activities and visual processing tasks occur naturally through play and experiencing the outdoors.
Try some of these outdoor activities to support the visual system:
- Play I Spy
- Hide objects and find them
- Play tag (visual tracking and visual scanning)
- Collect rocks or leaves (visual figure ground)
- Watch the clouds (visual attention)
- Look for birds
- Collect items from nature and notice differences
2. Proprioceptive System- Another of the “Big 3” sensory systems (explained in detail in our book, The Sensory Lifestyle Handbook), is the proprioceptive system.
There are so many proprioceptive activities supported by the outdoors. Try some of these:
- Hike of inclines or declines
- Animal walks in the grass
- Relay races
- Pound and smash ice
- Lift and carry rocks or logs
3. Vestibular System- The vestibular benefits of slowing swaying side to side on a tree vine can organize the child who is challenged by sensory overload.
Try these outdoor vestibular activities:
- Make an outdoor balance beam
- Bend an pick flowers
- Play in streams
- Play backyard games
- Swing or play on playground equipment
- Roll on hills
- Climb up the slide
- Take the sensory equipment outside and use a sensory swing outdoors
4. Interoceptive System- There is a connection with interoception, too. This sensory system is responsible for hunger, thirst, fatigue, digestion, sleep, toileting, and other internal systems. Sensory activities like going outdoors, experiencing differences in temperature and texture (warmth of the sun, cool breeze, wet rain drops, damp soil, etc.) on the skin receptors can impact how we feel, how mindful we are, and how the interoception system responds.
Outdoor sensory activities that impact the interoceptive system include:
- Running/walking/crawling
- Playing in wet sand, soil, grass
- Feeling the breeze on skin
- Feeling the warmth of sun on skin
- Playing on swings
- Going up or down a slide
- Laying on the ground (pressure on the stomach and internal organs)
- Rolling on the grass (vestibular and proprioceptive systems)
5. Auditory System- Outdoors, you can rest your state of mind just by listening. The outdoors offer a great mindset strategy for emotional regulation and is a way to calm the body. These backyard auditory processing activities will get you started. Try these outdoor auditory processing strategies for regulation and sensory needs:
- Listen for birds
- Mimic sounds
- Play “I hear” (just like I Spy for sounds)
6. Tactile System- The outdoors offer so many tactile experiences. From walking in grass without shoes on, to playing the variety of natural tactile sources, there are so many ways to support the tactile system outdoors.
Try some of these calming or alerting sensory activities for the tactile sense:
- Walk barefoot in grass
- Play in a sandbox
- Climb a damp tree
- Pick grass
- Dig in dirt
- Play with messy, sensory play outside
- Pick flowers
- Feel and crunch leaves (also great for the auditory sense)
- Create a tactile nature walk collection
7. Gustatory System- The gustatory sense, or the sense of taste can be incorporated into the outdoors. Think about your experience with picking berries, tasting a cool and sweet popsicle on a hot day. There are so many sensory-based memories involving tastes. Try some of these gustatory sensory activities in the outdoors:
- Grow a sensory garden with fruits and vegetables that can be eaten outdoors
- Eat a juicy watermelon outside- This is a great tactile activity, too
- Make ice pops, smoothies, or ice cream using fresh fruits.
9. Olfactory System- This is the sense of smell. Outside, there are so many scents that occur and may change every day (and even based on the time of day!) Consider these olfactory sensory ideas:
- Smell flowers
- Smell grass
- Identify odors and scents by location
- Name the type of plant based on scent
- Garden- Plant herbs such as mint, parsley, basil, lavender, etc. These are powerful scents that can be calming.

Outdoor Sensory Play
There are so many outdoor activities that incorporate play naturally while meeting underlying needs in the great outdoors! The ideas you’ll find below are naturally occurring play ideas using items found in nature, natural environments. They are outdoor activities that kids can try without any additional equipment or specialty therapy items.
The point with these outdoor occupational therapy strategies is to support motor skill development, motor planning, visual motor skills, and overall development through the natural environment of the outdoors.
Ideas for outdoor occupational therapy:
- Hike
- Play in the woods
- Roll down hills
- Balance beam on logs
- Climb trees
- Collect nature
- Play at the beach
- Nature walk
- Play in the backyard
- Climb on stumps
- Jump in puddles
- Driveway or pavement play activities
- Swing on tree vines
- Sensory play on a porch or enclosed space
- Collect sticks
- Leaf hunt
- Water table
- Move and carry rocks of various sizes
- Hide and seek
- Create with nature
- Outdoor water play
- Collect fireflies
- Pour rocks
- Build with rocks, stumps, sticks, small logs
- Mix and create nature soup (mud, sticks, flower petals, grass clippings)
- Mud play
- Use more of the ideas in our Outdoor Sensory Diet Cards
The outdoor world is full of sensory input that can meet individual needs of every child. The kids with sensory needs as well as those who present as neurotypical will benefit from a lifestyle of sensory play and experiences in the outdoors.
As always, these activities should be looked over and utilized along with assessment and intervention of an occupational therapist, as each child differs so very vastly.
Some of the ideas above are going to be described in more detail here on The OT Toolbox. Watch this space for more outdoor sensory play ideas based on the following outdoor play spaces:
- Backyard Lawn Sensory Diet Activities
- Wooded Areas Sensory Diet Activities (Perfect for a camping trip or playing in the woods at home or at a park!)
- Playground Sensory Diet Activities
- Beach Sensory Diet Activities (Perfect for a family vacation to the beach or for those who live near a beach area!)
Sensory diets and specific sensory input or sensory challenges are a big part of addressing sensory needs of children who struggle with sensory processing issues.
Incorporating a schedule of sensory input (sensory diet) into a lifestyle of naturally occurring and meaningful activities is so very valuable for the child with sensory needs.
That’s why I’ve worked to create a book on creating an authentic and meaningful sensory lifestyle that addresses sensory needs. The book is now released as a digital e-book or softcover print book, available on Amazon.
The Sensory Lifestyle Handbook walks you through sensory diet creation, set-up, and carry through. Not only that, but the book helps you take a sensory diet and weave it into a sensory lifestyle that supports the needs of a child with sensory processing challenges and the whohttps://www.theottoolbox.com/product/the-sensory-lifestyle-handbook/le family.
Get The Sensory Lifestyle Handbook here.