Today, we’re covering problem behavior in preschoolers, including behaviors that impact learning and development because of participation in preschool activities. Every preschooler, family, and classroom is different. With the uniqueness embedded into an Early Childhood Classroom, it isn’t uncommon for teachers to have some run-ins with concerning behavior. This blog will teach you the five steps to creating a behavior plan for managing preschool behaviors, which encourages positive interactions with parents and children.
The uniqueness of every family and child plays a role in each preschool classroom. Every teacher has expectations. All classrooms are set up differently, and the environment can change, based on the activities and people who are present. Understanding how to support children and their families, while teaching children academic, social, and emotional skills, can be daunting for preschool teachers.
examples of challenging preschool behaviors
Some of examples of challenging behaviors in preschoolers include:
- Hitting, scratching, slapping, grabbing
- Biting, spitting, chewing on non food items, licking
- Kicking others
- Bolting out of the classroom or other setting
- Refusing to work, refusal to cooperate, talking back
- Yelling, screaming, crying
- Tantrums – Check out this post on the OT Toolbox to better understand meltdown vs. tantrum behavior
This is just the tip of the iceberg. Do any of these behaviors sound familiar?
What causes challenging behaviors in preschool?
Before covering strategies to address behaviors that impact learning and the development of skills, it is important to understand why we may see challenging behaviors in the preschool setting.
Based on these Kindergarten readiness standards of emotional readiness, 5-6 year old children are expected to know how to calm down, listen to teachers, follow directions, take turns with peers (this is a great resource on turn taking), and transition between activities throughout the school day.
When a child enters preschool, they typically haven’t had much experience with some of these tasks. Some young children adapt well to the social and emotional expectations of a large group situation, while other children need extra support.
Behavior Triggers
There can be a multitude of reasons why problem behaviors occur in the preschool setting. Just some of the behavior triggers that lead to common issues in the preschool setting include these causes:
- Having a new routine (potty training, time change, or differing work schedules of parents are some examples) throws off the child’s ability to self regulate
- Experiencing a change in home environment (a new baby added to the family, moving to a new home, or other home changes)
- Not getting enough sleep (check out this article on sleep hygiene)
- Too much screen time
- Developmental changes in the preschool age range
Breaking these underlying areas down, it is possible to see three common factors that may trigger a behavioral response between the ages of 3-5 years.
As a related read, check out our fine motor activities for preschoolers as a way to support development during the yearly childhood stage.
Common causes of preschool behaviors
There are three common causes behind preschool behaviors: basic needs need met, environmental issues, or the behaviors of others (peers). Let’s explore each of these common causes of preschool behaviors.
Three common triggers of preschool behavior outbursts:
- Basic needs (hunger, sleep, thirst, temperature) Is the child hungry, tired or overwhelmed? Is it close to snack time or nap time? Did the child drink enough water while they were playing outside? Basic needs affect everyone differently. Children tend to be sensitive to bodily changes. Medical issues may affect basic needs. Make sure to be in contact with parents about any sort of change in a child’s health. This includes toileting challenges (constipation), new medications they may have been given, and allergy concerns.
- Environment (changes to routine of the environment, home situation, transportation, changes to the classroom environment: lights, sounds, smells, temperature, distractions, unexpected changes).
- Behavior of others (behavior of peers, behaviors and actions of adults, parents, caregivers, educators, and behaviors of others in the classroom: other children making noise, someone provoking them, someone else having a tantrum). These friendship activities for preschool can help with this area of social emotional learning.
Triggers of challenging behavior in the preschool age range can be compounded by several of these considerations occurring at one time. Additionally, preschoolers can struggle with communication to let others know what is happening in their world.
How to support challenging preschool behaviors
Children learn best from consistency. This pertains to social and emotional expectations, both at home and in the classroom.
Talking to families about concerns regarding their child’s behavior, is one of the hardest conversations that a teacher can have.
By creating a 5 step behavior plan with the family, educators can support children, while also demonstrating to families that they are there to help by teaching their child how to interact and engage with their peers.
5 Step Behavior Plan for Preschoolers
Here are the 5 steps to complete when creating a behavior plan for a child. Going through these steps, you’ll see that addressing emotional regulation, getting to the root of underlying causes and considerations, creating an age-appropriate plan, including play-based strategies or tools to support development in these areas.
As always, the concept of the “iceberg” of underlying considerations is upheld.
1. Determine the cause of the behavior
There are many different causes of a child’s behavior. Parents and teachers can track the behavior of a child, gathering data using an ABC chart. This refers to antecedent (what happened before the behavior started), behavior (what that child did), and the consequence (how did the child and adult respond to the behavior.)
When observing children to understand the cause of their behavior, make sure to pay close attention to the common behavior triggers addressed and listed above. Getting clear on what’s causing the visible behavior is essential.
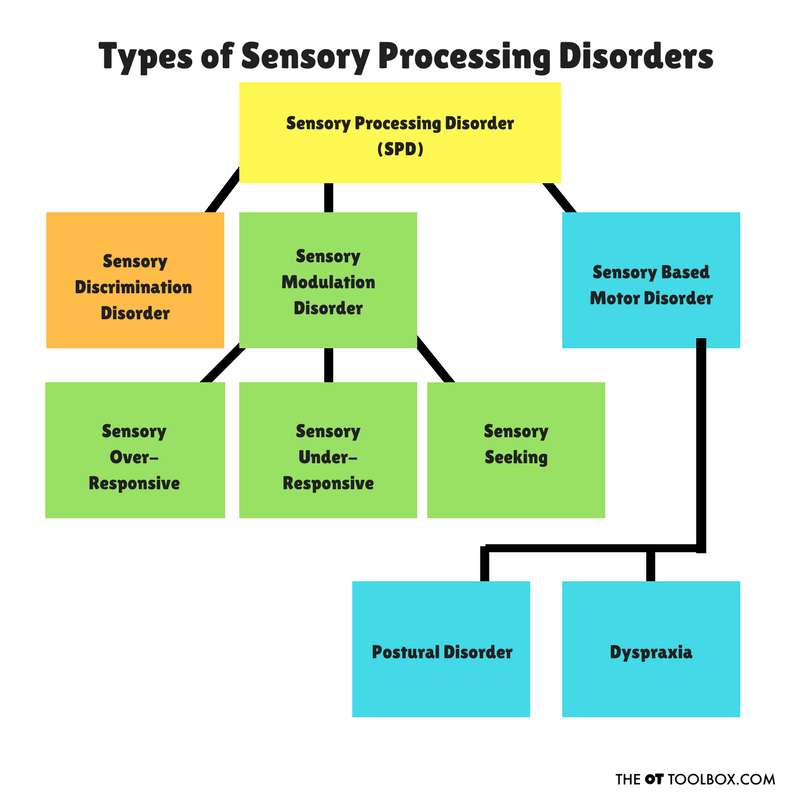
*Keep track of children that are known to have sensory sensitivities (Here are some questions to ask yourself when monitoring the environment:
- Have you changed anything in the room?
- Has the weather been different (humid, rain, snow, extra cold or hot)?
- Is it really bright and sunny, or gloomy and foggy?
- Does the child have any sensory sensitivities such as clothing, sounds, being touched?
- Have you changed the classroom routine?
- Has the child touched or engaged in a sensory rich experience they may not have liked (finger-paint, sensory bin, slime, play dough)?
- Is the classroom too loud or very busy?
- Check if the child is wearing something new/uncomfortable (do their shoes fit? Is there a scratchy tag on their clothes? Is their diaper too tight?)
- Here is a great post on working with children with sensory differences.
2. Talk to parents and caregivers
Once you have narrowed down the cause of the behavior, make a plan to meet with the child’s caregivers (parents, grandparents, daycare staff) to go over your findings. Include any member of their team who spends a great amount of time with this child.
Documented evidence and observations from the ABC chart will give you concrete examples of what is happening, and why.
When starting the conversation with the family, begin by describing the child’s strengths. Share their child’s favorite activity to do at school, who their friends are, and one great thing they did that week.
Next, show the family the ABC chart, explain what behaviors you want to change, and what new behaviors you would like the child to do instead.
Encourage the family and other caregivers to share their observations of the child at home, and out in the community.
3. Create goals to improve preschool behaviors
After sharing what you are going to work on with their child, include the team in goal setting, allowing caregivers to share what they would like their child to do. As you write these goal, phrase the goals in a positive way, showing what you expect from the child.
As with all goals, make sure they are measurable and attainable. For goal setting tips, check out this post on using a goal ladder.
Make an appointment for a follow up meeting with the family, so you can check in on how the child is doing at home, at school, and out in the community.
For example:
- Jackie will use her words when she wants to use a toy 80% of the time.
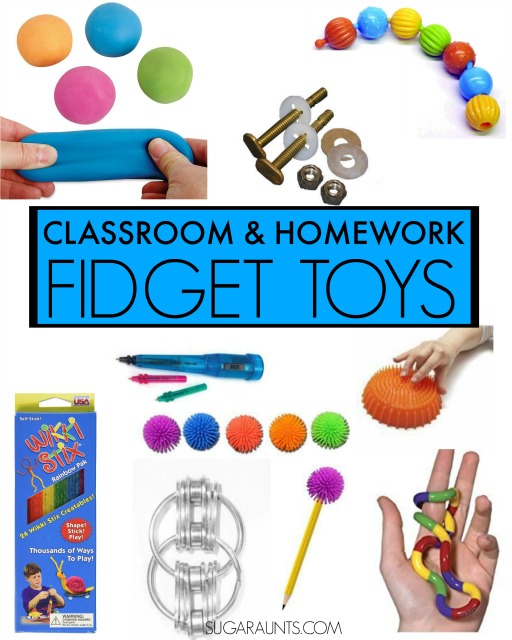
- Mark will participate in circle time for 10 minutes with supports such as breaks, sensory fidgets, alternative seating without leaving the area.
- Trent will transition from outside to inside time on her own without maladaptive behaviors or needing to have physical support.
Next, it’s time to come up with a way to support the child in meeting these goals.
4. Establish interventions for challenging preschool behaviors
As you determine the interventions to be used at school, share them with the family, encouraging them to use the same interventions at home and in the community.
Children thrive on consistency. When receiving the same messages and intervention techniques at home and school, children will learn the behavior faster. They will learn to carry over the behaviors from one setting to the next.
Three common interventions to include in a preschool behavior plan:
- Create a calm down corner with tools for emotional regulation- Children tend to become overwhelmed, losing control of their emotions, when they don’t have a positive way to calm down. Soothing Sammy teaches children how to calm down, using visual and tactile tools, while supporting a positive image of feelings. As children learn how to manage their feelings, they are able to communicate and problem solve in different situations.
- Sensory diet for the classroom – When children become frustrated due to sensory difference, a sensory diet for the classroom and home works wonders, by giving children the tools to cope with their struggle. This list, created by occupational therapists, includes practical strategies easily implemented in any preschool classroom.
- Utilize Visual and Auditory Cues for Transitions- Children who are overwhelmed or frustrated, don’t always hear what others are saying to them. These transitions for children can be a challenge. The use of visual schedules, visual prompts, and auditory cues remind children what is expected of them, when they aren’t able to process what is said. Using visual tools such as a picture schedule, first/then chart, or picture exchange cards (PEC), while keeping directions clear and simple can help. Adding an auditory prompt, such as a bell or clapping, to signify it is time to clean up, gives children multisensory ways to receive a direction.
- Try calm down toys based on the child’s interests.
Check out this visual cue resource for use in daily activities, sensory diets, PECs, and visual supports.
5. Preschool Behavior Plan Follow through
When following through with a preschool behavior plan, the next steps are important. This follow through looks like many things.
Talking with parents and caregivers, make sure that you follow up with a second meeting to discuss the child’s progress. This is important, as it gives the parents the ability to weigh in on the next steps, the teachers to provide parents with constructive feedback of how their child is doing, and an opportunity to discuss a referral to specialists if needed.
Some of the most common specialist referrals are:
- Audiologist for a hearing evaluation
- Occupational therapist for sensory, behavior, motor skill concerns
- Speech therapist for language delays
- Early Intervention for developmental delays
- Behavior therapist for more intensive behavior needs
- Pediatrician for concerns about medically based delays (including autism, ADHD, nutrition, sleep, or gastrointestinal issues)
- Note: teachers need to be cautious when suggesting referrals to other professionals, offering possible diagnoses, or alarming caregivers.
check out these other great resources from the OT Toolbox to support behavior
- attention and behavior problems
- movement breaks and behavior
- how to support self regulation in preschoolers
- problem solving activities for preschoolers
- emotional vocabulary for preschoolers
Creating a behavior plan helps parents and teachers work together regarding preschool behaviors. Providing an environment that includes consistency, open communication, and sensory supports, will give every child a supportive environment they need to thrive. This five part behavior plan blueprint includes strategy ideas, goal creation tips and resources for behavior tracking. A behavior plan is an essential component of a healthy classroom.

Jeana Kinne is a veteran preschool teacher and director. She has over 20 years of experience in the Early Childhood Education field. Her Bachelors Degree is in Child Development and her Masters Degree is in Early Childhood Education. She has spent over 10 years as a coach, working with Parents and Preschool Teachers, and another 10 years working with infants and toddlers with special needs. She is also the author of the “Sammy the Golden Dog” series, teaching children important skills through play.