In this blog post, we are covering therapy for picky eaters. Occupational therapists and speech therapy practitioners often cover extremely picky eating in therapy sessions, but how do they know where to begin with food therapy? Let’s cover specifically how to help extremely picky eaters, food for picky eaters, and therapy suggestions for extremely picky picky eating disorder.
Therapy for Picky Eaters
Fifty years ago, feeding therapy this would not have been a popular topic. Children ate what was provided, like it or not. Sometimes parents would spare the child and leave the offending objects off of the plate. More often than not, children over the age of four were expected to eat what everyone else was eating.
Fast forward to 2022. There has been a huge rise in allergies, picky eaters, and problem feeders. How to help extremely picky eaters has become the forefront of many occupational therapy sessions and referrals.
There has been a marked rise in food sensitivity (gluten intolerance, lactose intolerance) or allergies to certain foods. This goes hand in hand with the rise of anxiety, illness, ADHD, autism, and poor immune response.
Picky Eater List
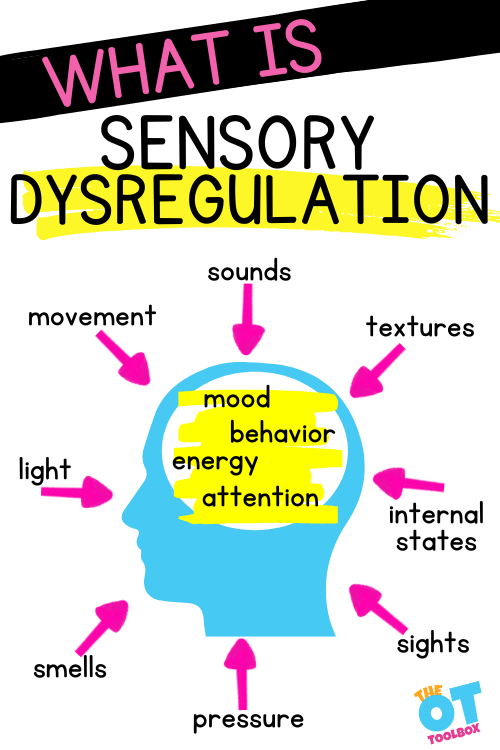
There is a difference between oral motor skills that impact feeding abilities and a child’s picky eating. Foods that make the “picky eater’s list” might include certain food texture issues, food mixtures, food sensory issues like crunchy foods, and even foods that require utensils.
A short list of some foods that are not on the plate of extremely picky eaters might include:
- Sandwiches
- Rice
- Chicken breast or other meats
- Carrots
- Cheese
- Sauces
- Vegetables
- Fruits
Obviously this is a short list and any number of foods, food types can be on a picky eater list. Any other number of foods or food combinations
Looking at this list, you can see the limitations in nutrients, vitamins, proteins, and brain-building foods that are missing from the plate of an extremely picky eater.
It is not productive to get stuck in the “why is my child a picky eater”, but move forward to “what can I do about picky eating”. I am not just an experienced feeding therapist, I too had two picky eaters who survived on 3-4 different foods in their second and third year of development.
In order to help my daughters, I had to remove my thoughts impacting how I approached tackling that picky eater list for each child. That includes putting aside parenting/worry/anxiety/they’re starving persona, and put on my therapist hat. I am happy to report they are thriving adults who eat a huge variety of foods!
NOTE*The term, “learner” is used throughout this post for readability and inclusion. Not all picky eaters are children. This information is relevant for students, patients, clients, preschoolers, kids/children of all ages and stages or whomever could benefit from these resources. The term “they” is used instead of he/she to be inclusive.
How to help extremely picky eaters
To learn how to help extremely picky eaters, it is important to define it first.
Picky eating is different from problem feeding. Often, but not always, extremely picky eating is actually a problem feeding disorder. This has recently been renamed Avoidant Restrictive Food Intake Disorder ARFID. ARFID is not classified with eating disorders such as anorexia and bulimia, as persons with ARFID or problem feeding do not restrict their intake due to body image.
The term picky eating includes:
- Selective eating habits
- Eats 10-20 different foods (preferred foods)
- Will often eat more if hungry
- Not missing entire food groups
- Can often be bribed or rewarded for good eating
- Can be distracted into eating
- Adds new foods to their diet
Problem feeding (extremely picky eating) refers to:
- Refusal to eat
- Rigid eating habits (no food touching, specific brand, same plate, cut a certain way)
- Eats less than 10 different foods
- Will starve before they eat unwanted foods
- Missing entire food groups
- Behavioral reactions: gagging, vomiting, crying, anxiety, refusal to sit at the table
- Increased sensitivity to the taste and/or texture of foods
- No amount of rewards, bribing, punishing will magically make this go away
- Does not recognize hunger
- Food jags, will lose foods once eaten regularly
What is the difference between picky eating and problem feeding?
The picky eater will survive. They are likely to consume at least one meat, fruit, and vegetable and a bunch of carbs.
Continue to put out expected foods on the plate and encourage tasting of new foods. The problem feeder on the other hand, is not consuming enough calories, or getting the right nutrition.
A person surviving on four foods often gets tired of one of them, eating only three foods now. This is more of a dire situation and the treatment is complicated.
If you have a problem feeder, seek treatment from a therapist who is certified or has attended classes in feeding therapy. There is a lot that can go wrong working with problem feeders.
The Sequential Oral Sensory course, Beckman Oral Motor Therapy, and Mealtime Miseries are popular courses. Having this information can help in identifying whether extremely picky eating is related to sensory or oral motor difficulties.
Therapy for Extremely Picky Eating
After viewing the list, if you feel the learner is more of a picky eater, there are several strategies that can help.
Following a feeding evaluation, feeding therapy can begin. Start a structured feeding problem including the following:
1. Feeding Therapy Interview
Interview the caregiver to determine the following:
- What foods the learner eats – a specific list will determine texture, variety, color, or patterns. Are all the foods crunchy? Are they all brown?
- How many foods the learner eats – less than 10 is a problem, 10-15 is picky, and above 20 is average. Count two different cookies as two items, two cereals as two items.
- Medical history – Is there a history of reflux, G-tube, or NG-tube, swallowing issues?
- Time frame for eating – A typical meal should last 20-30 minutes for a child.
- Where the learner eats – Does the learner eat at the table or in front of the television? Do they run around the room catching a bite here and there?
- Behavioral reactions during meal times – Does the child flee the table? Turn their whole body away from the food, vomit, cry, refuse to open their mouth, gag, spit out food?
Record information from caregivers and look for clues to feeding issues, other than the exhibited behavior. The person may have a history of reflux that makes eating very uncomfortable. They may have been verbally abused and shamed during mealtime, making eating an unpleasant experience. Perhaps the child has never had structure or routine during meal time, thus not making eating a priority.
2. Planning for Feeding therapy
Start treatment planning
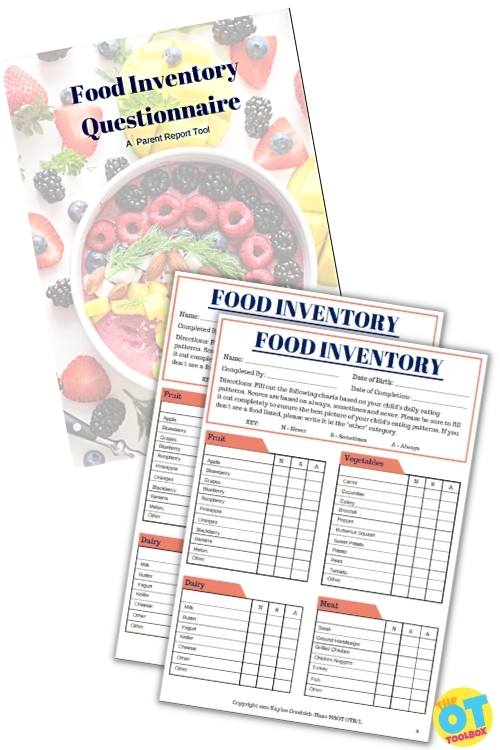
Begin with the provided list of preferred foods to determine what foods to try first. A Food Inventory Questionnaire can be used for this step.
If the learner eats: crackers, pancakes, waffles, bread, and dry cereal, they may have a preference for white/brown foods that are dry. Some are crunchy foods and some are soft foods, but all are dry.
The next in order would be another dry brown food such as toast, bagel, cookie, or different type of cracker.
Once the child tolerates more brown dry foods the next texture in the same color family would be a banana or plain macaroni.
For the learner who eats only purees or smooth foods like pudding, yogurt, and baby food, the next step would be to try different flavors of yogurt or pudding. For a learner who only eats smooth foods, it is important not to vary the texture yet. After the child tolerates this texture, then a trial of applesauce may work.
Adding flavor choices and additional nutrients can be found in sauces or dips. While this can be a source of refusal for some kids, others prefer dips such as ketchup or ranch dressing.
Take a look at what the individual is gaining from these dips. Both can be high in sodium and that salt intake is preferred. Can you offer other foods to dip into the preferred choices?
Think about other similar options that may offer a similar sensory input through texture or taste:
- butter for pasta rather than sauces
- pizza sauce in place of ketchup
3. Feeding Therapy Treatment session
Ask the learner or their caregiver to provide two favored foods and 2-3 non favored foods. Having preferred foods decreases anxiety as the child is not presented with a plate of non favored foods.
It is important for the learner/caregiver to provide the food. Possible allergic reactions are diminished, as the caregiver is more aware of the learner’s diet. There may be cultural or dietary foods that the family prefers.
It doesn’t do any good for the therapist to work for weeks on waffles and applesauce, if the family does not offer these foods.
Food presentation – Present all foods on the plate in small portions, or a choice of two options with small bites of each. Avoid huge piles of non-preferred food, as it increases anxiety or sensory aversion.
Divided plates help ease anxiety, as do small portions. It can help to present the food as snacks, using a snack plate or small tea plate.
Food exploration- Start to encourage eating, or at least food exploration. Have the learner look at the food, touch the food, touch it to their face, give a kiss, give a lick, take a bite, chew, and swallow. This resource on sensory touch can offer more information and strategies to support tactile exploration.
There are 27 steps to eating from being in the same room as the food, to chewing and swallowing it. This makes learning to eat new foods challenging.
Offer food options- Allow the child to touch foods or use their fingertips to pick up and eat or taste the foods. In some cases, muscles and coordination are not appropriate for utensil use, limiting options.
Read about suggestions to improve how to hold a spoon and fork.
Offer various food temperatures. Consider the sensory input offered by cooked carrots vs. raw carrots.
Offer various food cuts. Consider the amount of force needed to bite baby carrots vs. shredded carrots.
Food Therapy Progression
Food therapy interventions are about progressing through with small incremental changes to food offerings with observation and food challenges. Some food therapy goal banks are included below.
Learner is able to:
- Be in the same room as the food, then in the same area as the food.
- Sit near the food, then in front of the food without turning away.
- Look at food, touch the non preferred item, smell the food.
- Touch the food to face, then lips, then give it a kiss.
- Lick the food, take a bite and spit it out, chew the food with the option to take it out.
While presenting and working on the feeding portion, observe for signs of oral motor issues that might indicate oral motor development considerations.
- Does the learner chew from side to side or munch up and down?
- Do they have good lip closure?
- Do they have an intense gag reflex?
- Can they move the food around effectively?
- Can they bite into the food?
4. Carryover of Therapy for Picky Eaters
The ultimate goal is to carryover skills achieved in therapy sessions into a functional environment. Discuss techniques with caregivers and encourage them to try the same foods later in the day.
Remind them to be calm and not emotional during feeding time. The goal is to have fun with food and find mealtime enjoyable.
For more information on how to help extremely picky eaters, I have also published a helpful resource book (Amazon affiliate link) Seeing your Home and Community with Sensory Eyes for to understand different environments that may be impacting the eating habits of your child/clients, including the cafeteria, kitchen, restaurants, and more.
Feeding and toileting are two of the most frustrating, anxiety producing stages of childhood. Children start to exert their free will at this stage and can no longer be forced to do certain things.
Encourage parents, educate yourself on this topic, and spread the word, so problem feeding does not continue to rise along with other scary diagnoses.
This post is part of a series on feeding disorders/picky eating. Other resources you will find helpful include:
- How to do a Food Evaluation
- What you Need to Know About Sensory Food Issues
- Food Texture Issues and Sensory Aversions
- Oral Motor Problems and Feeding

Victoria Wood, OTR/L is a contributor to The OT Toolbox and has been providing Occupational Therapy treatment in pediatrics for more than 25 years. She has practiced in hospital settings (inpatient, outpatient, NICU, PICU), school systems, and outpatient clinics in several states. She has treated hundreds of children with various sensory processing dysfunction in the areas of behavior, gross/fine motor skills, social skills and self-care. Ms. Wood has also been a featured speaker at seminars, webinars, and school staff development training. She is the author of Seeing your Home and Community with Sensory Eyes.